by Bryce Williams, DDS, Oral and Maxillofacial Surgeon
Jim is a 42-year-old male who has been struggling with obstructive sleep apnea since he was diagnosed 8 years ago. He has tried CPAP, however, he removes it within the first hour of sleep and no modifications to the mask fit or machine type has improved his compliance. His greatest success was losing weight. He initially improved his BMI from 33 to 27, and has kept the weight off for three years. Regrettably, this only improved his apnea-hypopnea index (AHI) from 72 to 64. His sleep medicine physician, a pulmonologist who you are well acquainted with, referred him to your office for a mandibular advancement device, which you fabricated and delivered to the patient a few months ago. The patient has had improved compliance with the jaw advancement splint, wearing it throughout the night, most nights. His wife reports softening of his snoring, and the patient says he thinks he feels a little less tired during the day. The entire treating team considers this a success and his sleep medicine physician schedules a follow up polysomnography to quantify the amount of improvement that Jim has had. Unfortunately, the repeat polysomnography shows minimal improvement in the patient’s AHI, decreasing from 64 per hour to 51 per hour. The sleep medicine physician calls you to see if you have any additional recommendations for treatment. In your opinion, the device has advanced the jaw as far anteriorly as possible. The patient is becoming frustrated, but is willing to try something more invasive if it will improve his symptoms and prevent future systemic disease. What could you offer this patient?
Failure of conservative therapy in patients with severe sleep apnea (AHI > 30) is disappointingly common, with 20-40% rejecting treatment with CPAP, and up to 30% failing treatment with a mandibular advancement splint. For these patients, finding an acceptable treatment can be challenging. Surgery may appear to be an attractive option to the patient, as it is may be perceived as an instant solution to their disease that does not involve wearing awkward or restricting medical devices. To the contrary, most medical and dental providers know that surgery for sleep apnea has a reputation of being very painful with disappointing results. The reputation isn’t unfounded – a systematic review of patients with severe sleep apnea undergoing soft palate surgery had a 33% reduction in their AHI, but the mean post-op AHI remained 29 after surgery.1
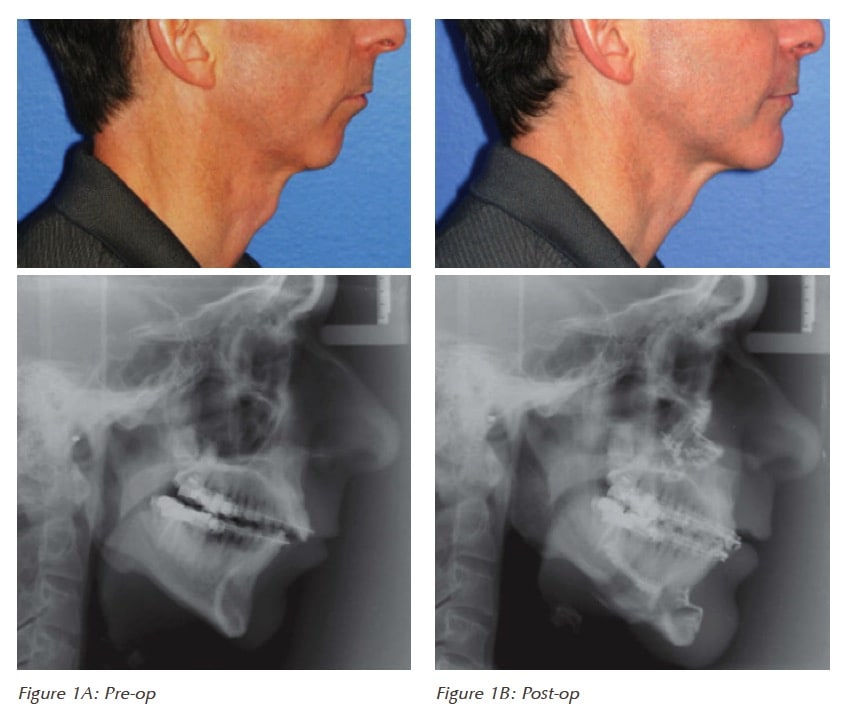 Jaw surgery (also called “orthognathic surgery”) for sleep apnea can consist of a variety of surgical designs. The most successful orthognathic surgery type for severe obstructive sleep apnea is maxillomandibular advancement surgery (MMA), which averages around a 90% reduction in AHI post-operatively. The surgery involves creating an osteotomy in the upper and lower jaws and the chin, and advancing the jaws anteriorly. This movement not only opens the airway in the anterior-posterior dimension, but also expands the airway laterally which is key for preventing collapse of the airway in patients with severe disease. Traditionally, orthognathic surgery is utilized in younger patients with a malocclusion – to correct an overbite or underbite, for example. In contrast, maxillomandibular surgery (MMA) is anterior repositioning of the jaws, usually in older patients, with the primary goal of expanding the airway. Oftentimes, these patients have a normal occlusal relationship, so that MMA surgery positions the jaw in an extreme anterior post-operative position. Despite the new, exaggerated anterior position of the jaws and chin, >90% of patients are very pleased with their post-surgery appearance as advancement of the jaws tightens facial wrinkles and produces a younger looking convexity of the face.2 Patients with pre-op mandibular retrognathia tend to have an anatomic cause for sleep apnea, and have the most esthetically pleasing and greatest airway expansion with maxillomandibular advancement surgery (see an example in Figure 1).
Jaw surgery (also called “orthognathic surgery”) for sleep apnea can consist of a variety of surgical designs. The most successful orthognathic surgery type for severe obstructive sleep apnea is maxillomandibular advancement surgery (MMA), which averages around a 90% reduction in AHI post-operatively. The surgery involves creating an osteotomy in the upper and lower jaws and the chin, and advancing the jaws anteriorly. This movement not only opens the airway in the anterior-posterior dimension, but also expands the airway laterally which is key for preventing collapse of the airway in patients with severe disease. Traditionally, orthognathic surgery is utilized in younger patients with a malocclusion – to correct an overbite or underbite, for example. In contrast, maxillomandibular surgery (MMA) is anterior repositioning of the jaws, usually in older patients, with the primary goal of expanding the airway. Oftentimes, these patients have a normal occlusal relationship, so that MMA surgery positions the jaw in an extreme anterior post-operative position. Despite the new, exaggerated anterior position of the jaws and chin, >90% of patients are very pleased with their post-surgery appearance as advancement of the jaws tightens facial wrinkles and produces a younger looking convexity of the face.2 Patients with pre-op mandibular retrognathia tend to have an anatomic cause for sleep apnea, and have the most esthetically pleasing and greatest airway expansion with maxillomandibular advancement surgery (see an example in Figure 1).
Jaw surgery may be viewed as a very major surgery. In actuality, there have been no reported deaths in the literature after maxillomandibular advancement surgery. Major complications are considered to be rare (<1%) and minor complications (3%) are very uncommon and are temporary and reversible.3 The numbness that occurs of the lips, chin and cheeks is not especially debilitating for the patient and is temporary in >85% of patients. The <15% of patients that have permanent numbness usually only have a very small area of the cheek or chin that is numb, and is not particularly incapacitating to the patient. The transient numbness has the paradoxical advantageous effect of decreasing the severity of post-op pain, which is why MMA is generally considered less uncomfortable compared to a less invasive surgery such as isolated soft palate surgery.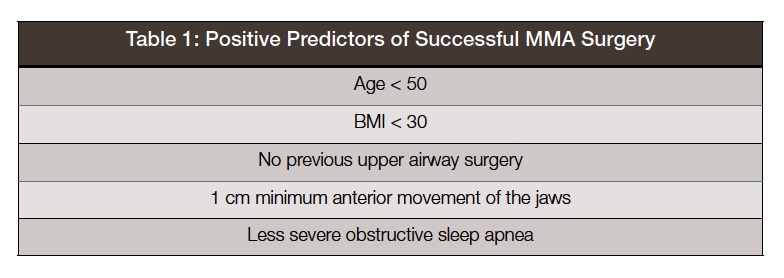 Which patients should be considered for maxillomandibular advancement surgery? The ideal patient has failed conservative treatment (CPAP, mandibular advancement device/splint), has a craniofacial deformity such as mandibular retrognathia, has a BMI < 30, is less than 50 years old, and has moderate to severe obstructive sleep apnea – similar to our patient Jim, introduced in the story above (see Table 1 highly positive predictor for MMA post-op success). Not every patient fits into the “ideal” patient categories listed above. Maxillomandibular advancement surgery is still considered one the most effective and safe upper airway surgery for patients with moderate to severe sleep apnea that have failed conservative treatment. This can include heavier patients who have had previous upper airway surgery that are > 50 years old. The reason is MMA surgery seems to result in the greatest overall reduction in AHI compared with other upper airway surgeries, so even more difficulty patients can qualify. These patients in the severe category of sleep apnea with difficulty complying with conservative treatment or failure of previous surgical therapies can and should, at least, be evaluated for maxillomandibular advancement surgery as they can have drastic improvements in symptoms, quality of life and AHI.
Which patients should be considered for maxillomandibular advancement surgery? The ideal patient has failed conservative treatment (CPAP, mandibular advancement device/splint), has a craniofacial deformity such as mandibular retrognathia, has a BMI < 30, is less than 50 years old, and has moderate to severe obstructive sleep apnea – similar to our patient Jim, introduced in the story above (see Table 1 highly positive predictor for MMA post-op success). Not every patient fits into the “ideal” patient categories listed above. Maxillomandibular advancement surgery is still considered one the most effective and safe upper airway surgery for patients with moderate to severe sleep apnea that have failed conservative treatment. This can include heavier patients who have had previous upper airway surgery that are > 50 years old. The reason is MMA surgery seems to result in the greatest overall reduction in AHI compared with other upper airway surgeries, so even more difficulty patients can qualify. These patients in the severe category of sleep apnea with difficulty complying with conservative treatment or failure of previous surgical therapies can and should, at least, be evaluated for maxillomandibular advancement surgery as they can have drastic improvements in symptoms, quality of life and AHI.
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..