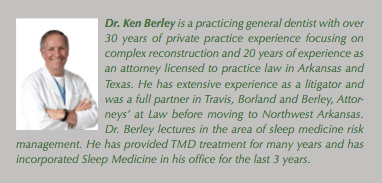
by Ken Berley DDS, JD, FAGD, FICOI
I bet you have never spoken to an attorney that understood what you go through on a daily basis and could identify with your struggles. Without understanding the plight of practicing dentists, it is hard for an attorney to be an effective advocate. Generally, attorneys don’t know how or what to do to help a dentist.
Therefore, the typical strategy applied by most attorneys is to help you get out of trouble, not prevent the calamity in the first place. I am a licensed attorney in Arkansas and Texas, but most importantly, I am a wet fingered dentist with over 30 years of dental experience. Just like you, I go to my dental office each morning. So, I understand what you are going through and I am on your side! It is my personal goal in this quarterly column, to keep YOU out of trouble! How am I going to do that, you ask? In every article I will discuss an issue in sleep medicine that is bothering me from a legal prospective. If it bothers me as a DDS/JD, trust me, it should bother YOU! Let’s fix the problem before a lawsuit is filed not afterwards!
Good attorneys are paid well to worry. They spend countless hours playing the “what if game!” It is a well known fact that everyone wants to avoid all legal risk, but unfortunately, if you own a car, home, business or practice any profession, avoiding all risk is impossible. The concept of risk management was birthed as a result of the “what if game.” What if: one of my sleep patients’ falls asleep while driving, can I be sued? What if: one of my patients’ complains to Medicare, what are my risks? What, if anything, can Medicare do to me? What if: one of my patients complains to the State Board of Dental Examiners, what is my true scope of practice and what are my legal rights? What if: I end up in court defending a malpractice claim; could a Sleep Physician testify against me regarding my (dental) standard of care? In this column we will delve into the many areas where risk abounds in the Dental Sleep Medicine arena.
Rarely is an attorney given a forum to express his opinions without a face-to-face encounter with an opposing attorney dogmatically arguing the counterpoint with great zeal. However, I have been given a unique opportunity and permission, to pontificate to my heart’s desire in this quarterly column. I feel that I am equal to the challenge and accept this opportunity with open arms. This column provides me with a platform to voice my opinion and draw attention to those areas that concern me legally. So let the pontification begin!
 And for those who might not be familiar with the term pontificate it means to: “talk in a dogmatic and pompous manner. To pontificate properly, you need to be a know-it-all with very strong opinions and the urge to share them.” No definition could describe me better. As you are hereby and forever forewarned, and with that introduction, I will let the concerns of my inner being loose with reckless abandon. “Cry Havoc, and let slip the dogs of war!” To start the discussion, I want to address an issue that needs immediate attention. I personally don’t like, and don’t use, the AADSM Informed Consent! While the AADSM consent form is better than some that I have read, it is seriously flawed in two areas: (1) The AADSM Informed Consent does not provide a place for a witness to sign the document! It is imperative to have a witness sign the informed consent to identify the member of your staff that witnessed the patient sign the document. More importantly, you need to know who was present in the room with the patient answering any question the patient might have. You should have the witness (staff member) go over the document with the patient asking the patient if they understand each paragraph. You should establish this routine within your office so your witness can testify to the office policy and routine regarding obtaining informed consent. The witness (staff member) can testify to any specifics that they can remember about the patient in question, then back this up with details regarding office policy and routine. It is my office policy to personally question the patient about any lingering questions that they might have. When all questions are answered, I sign the document in the margin.
And for those who might not be familiar with the term pontificate it means to: “talk in a dogmatic and pompous manner. To pontificate properly, you need to be a know-it-all with very strong opinions and the urge to share them.” No definition could describe me better. As you are hereby and forever forewarned, and with that introduction, I will let the concerns of my inner being loose with reckless abandon. “Cry Havoc, and let slip the dogs of war!” To start the discussion, I want to address an issue that needs immediate attention. I personally don’t like, and don’t use, the AADSM Informed Consent! While the AADSM consent form is better than some that I have read, it is seriously flawed in two areas: (1) The AADSM Informed Consent does not provide a place for a witness to sign the document! It is imperative to have a witness sign the informed consent to identify the member of your staff that witnessed the patient sign the document. More importantly, you need to know who was present in the room with the patient answering any question the patient might have. You should have the witness (staff member) go over the document with the patient asking the patient if they understand each paragraph. You should establish this routine within your office so your witness can testify to the office policy and routine regarding obtaining informed consent. The witness (staff member) can testify to any specifics that they can remember about the patient in question, then back this up with details regarding office policy and routine. It is my office policy to personally question the patient about any lingering questions that they might have. When all questions are answered, I sign the document in the margin.
(2) The AADSM Informed Consent does not ask the patient for explicit consent. The only place in the form that uses the word “consent” is in the title of the document. Therefore, if you use the AADSM document you are relying on the doctrine of implied consent to provide treatment. In my “opinion, opinion, opinion” as my friend JT says, it is imperative for the patient to affirmatively agree and consent to the treatment. The last two paragraphs of the consent that I drafted for use in our office states as follows:
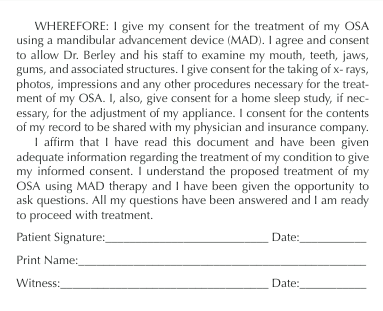 The informed consent document is your “get-out-of-jail-free card!” In my 34 years of practicing dentistry and 20 years of practicing law, I have never had a patient refuse to sign an informed consent. So why not use this document to the fullest extent possible. Put any and everything possible in this document. My Sleep Informed Consent mentions “DEATH” more than once. This form can be the document that stops a malpractice suit or at the very least, presents a significant obstacle to overcome in finding a dentist to be medically negligent.
The informed consent document is your “get-out-of-jail-free card!” In my 34 years of practicing dentistry and 20 years of practicing law, I have never had a patient refuse to sign an informed consent. So why not use this document to the fullest extent possible. Put any and everything possible in this document. My Sleep Informed Consent mentions “DEATH” more than once. This form can be the document that stops a malpractice suit or at the very least, presents a significant obstacle to overcome in finding a dentist to be medically negligent.
With that in mind, I am placing a copy of my sleep informed consent on my web site (DrKenBerley.com) if any of you are interested in downloading a copy. It does not have a copyright and you are free to adapt it to your needs. Additionally, please join me in encouraging the AADSM to modify this vital document.