
You may think your impact is limited to your patients, or to the doctors you work with. Think bigger, like Dr. Todd Morgan; one of the true pioneers of our field, and you might be part of shaping entire fields of medicine. His story begins with his early research and what he called the “Jaw Advancement Device.” As a busy clinician and patient advocate, he has continued to develop new design features and innovate calibration techniques for oral appliances.
He publishes regularly in peer reviewed journals, has authored book chapters and even entire illustrated books. His newest book, for children and parents, is Why the Long Face? A Book about Thumb Sucking1.
 Todd believes that much of the basis for understanding airway collapse hinges on early craniofacial growth and development. “It’s easy to understand why obesity can cause OSA, but what about other folks?” Todd went on to say: “The human pharynx is unique among mammals, and we’re lucky it’s floppy enough for speaking. But when muscles largely turn off in sleep we are also uniquely defenseless to collapse. This becomes especially true for those patients with the classic narrow arch form and high palate- a sign of a narrowed airway as well.” “They get quicker to collapse, or, they could have an inadequate neuromuscular response to that challenge.” “We are just beginning to understand really how oral appliances positively influence pharyngeal dynamics, and in whom. It’s not simple.” Todd invited me and our readers to read a chapter on phylogeny of the pharynx that he wrote with Dr. John Remmers if these concepts stir interest: Phylogeny and Animal Models: An Uninhibited Survey2.
Todd believes that much of the basis for understanding airway collapse hinges on early craniofacial growth and development. “It’s easy to understand why obesity can cause OSA, but what about other folks?” Todd went on to say: “The human pharynx is unique among mammals, and we’re lucky it’s floppy enough for speaking. But when muscles largely turn off in sleep we are also uniquely defenseless to collapse. This becomes especially true for those patients with the classic narrow arch form and high palate- a sign of a narrowed airway as well.” “They get quicker to collapse, or, they could have an inadequate neuromuscular response to that challenge.” “We are just beginning to understand really how oral appliances positively influence pharyngeal dynamics, and in whom. It’s not simple.” Todd invited me and our readers to read a chapter on phylogeny of the pharynx that he wrote with Dr. John Remmers if these concepts stir interest: Phylogeny and Animal Models: An Uninhibited Survey2.
His current research investigations are looking into the role of oropharyngeal exercise for OSA, and as a rehabilitation strategy for stroke sufferers with swallowing difficulties. Todd believes that myofunctional strengthening can play an important adjunctive role in improving outcomes for patients, and that patients are looking for self-help strategies.
 Outside his busy general dental and sleep practice, he has served in leadership roles for the AADSM for more than ten years, and is the current Chief of Oral Medicine at Scripps Memorial Hospital in Encinitas. He is the Dental Sleep Medicine consultant to Scripps Clinic Division of Chest Medicine in La Jolla, California, and currently serves on the Board of Directors of the California Sleep Society. Dr. Morgan also holds three patents on oral appliance design.
Outside his busy general dental and sleep practice, he has served in leadership roles for the AADSM for more than ten years, and is the current Chief of Oral Medicine at Scripps Memorial Hospital in Encinitas. He is the Dental Sleep Medicine consultant to Scripps Clinic Division of Chest Medicine in La Jolla, California, and currently serves on the Board of Directors of the California Sleep Society. Dr. Morgan also holds three patents on oral appliance design.
Todd’s Story:
After graduating dental school in 1986 I returned to San Diego, renting some space that was previously a dental office. While waiting for patients to stroll in I had time on my hands and read everything. One day I happened upon an anecdotal report on the “Snore Guard” invented by Tom Meade DDS, at the time being promoted by Tom and his colleague Wolfgang Schmidt-Nowara, MD. Out of curiosity I scheduled a time to meet with them. Well, once I understood a bit more, there was no stopping from then on. I was hooked!
 For lots of years after that I was creating my own version of the Snore Guard by gluing two night guards together – and having lots of success treating snoring and having a big impact on many of my patient’s lives. I was treating OSA but didn’t know it, and I wanted to learn more! So I took a chance and went to Scripps Clinic’s Sleep Medicine Department in 1990 with my acrylic creations. There I met Dr. Stuart Menn who engaged me and together we published (after 3 years of revisions and three sleep fellows) a sentinel article in the Journal SLEEP called: The Mandibular Repositioning Device: Role in the Treatment of Obstructive Sleep Apnea3. I feel very fortunate that I had a chance to collaborate and develop friendships with many of the leading experts in sleep medicine of our time, like Drs. Milton Erman, Merrill Mitler, Dan Kripke, Phillip Westbrook, Arthur Dawson, Steven Poceta and Dan Loube to name only a few. My tail has been on fire ever since then, yet I am excited to know that my adventure in learning, teaching and publishing in this field has yet only just begun.
For lots of years after that I was creating my own version of the Snore Guard by gluing two night guards together – and having lots of success treating snoring and having a big impact on many of my patient’s lives. I was treating OSA but didn’t know it, and I wanted to learn more! So I took a chance and went to Scripps Clinic’s Sleep Medicine Department in 1990 with my acrylic creations. There I met Dr. Stuart Menn who engaged me and together we published (after 3 years of revisions and three sleep fellows) a sentinel article in the Journal SLEEP called: The Mandibular Repositioning Device: Role in the Treatment of Obstructive Sleep Apnea3. I feel very fortunate that I had a chance to collaborate and develop friendships with many of the leading experts in sleep medicine of our time, like Drs. Milton Erman, Merrill Mitler, Dan Kripke, Phillip Westbrook, Arthur Dawson, Steven Poceta and Dan Loube to name only a few. My tail has been on fire ever since then, yet I am excited to know that my adventure in learning, teaching and publishing in this field has yet only just begun.
What Contributions Do You Feel You Have Made to DSM:
I feel like my largest contribution lies in my devotion to patient care. Saving lives is very cool. Secondary to that is research and teaching, which I’ve integrated into my patient care. It’s such a passion of mine that it’s hard to treat anyone without wondering “What I will discover with this case?” There is still a ton to uncover, all the way from patient selection to improved appliance design. I believe the key to success and best outcomes is finding the correct bite for the case right from the start. This is why we have worked hard to develop the Apnea Guard system, once we understood the importance of adding vertical height to the protrusive position.
We actually stumbled onto discovering the impact of vertical while conducting our NIH funded oral appliance outcome studies in the late 2000’s. Back then, we studied 130 patients using the TAP II and TAP III appliances and saw different outcomes when we dived patients by gender and which appliance was fabricated. The TAP II had significantly more vertical opening than the TAP III. When we retested a subset of our cohort and crossed over appliances we discovered that the male subjects did much better with more vertical opening. Once I understood when to use vertical my clinical result greatly improved in my practice. A bit later we decided to develop the Apnea Guard trial appliance that guides the user thru a simple algorithm for proper vertical selection in each case and the Apnea Guard is now growing in popularity for this reason, and because you can offer immediate treatment while the patient waits for their custom appliance. Based on our FDA trial that compared Apnea Guard to custom appliance outcomes4, we know that the Apnea Guard correctly predicts the correct protrusive and vertical jaw position and that that position can be transferred to the final customized device. I am very excited about the future of this technology.
I am currently focusing on the role of oropharyngeal exercise in treating OSA. Over the past five years some wonderful evidence has been published that shows this type of exercise can be very helpful. Everyone thinks about the Didgeridoo study published by Punan5 quite a while back when exercise for OSA comes up. That study was small and interesting, but it is largely impractical to buy and start playing one of these massive instruments. It is also interesting to ponder how circular breathing technique helps to strengthen the right muscles to defend against airway collapse.
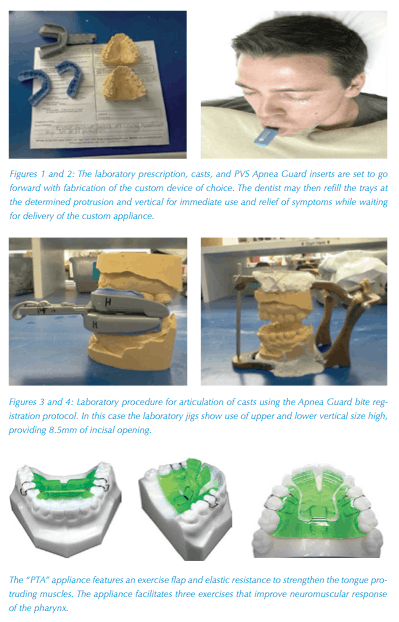 Then in 2009, a Brazilian investigator named Katia C. Guimaraes6 published a remarkable paper showing dramatic improvements in OSA in a group of 40 men with moderate OSA using speech therapy exercises and neuromuscular stimulation. I was so impressed I decided to study and better understand the actions of all of the pharyngeal muscles as well as the reflexes associated with tongue positioning. Through this effort I was able to design a novel device called the Pharyngeal Training Appliance (PTA), nicknamed the “Lifeguard.” Right now we are in the investigational stages of adding the PTA to our clinical protocol when oral appliance outcomes fall short of expectations. Early results are looking good. We also have the PTA started in a clinical trial for rehabilitation of stroke patients with swallow dysfunction7.
Then in 2009, a Brazilian investigator named Katia C. Guimaraes6 published a remarkable paper showing dramatic improvements in OSA in a group of 40 men with moderate OSA using speech therapy exercises and neuromuscular stimulation. I was so impressed I decided to study and better understand the actions of all of the pharyngeal muscles as well as the reflexes associated with tongue positioning. Through this effort I was able to design a novel device called the Pharyngeal Training Appliance (PTA), nicknamed the “Lifeguard.” Right now we are in the investigational stages of adding the PTA to our clinical protocol when oral appliance outcomes fall short of expectations. Early results are looking good. We also have the PTA started in a clinical trial for rehabilitation of stroke patients with swallow dysfunction7.
So, the future is wide open in my opinion. There is plenty to discover and develop in the field of Dental Sleep Medicine, including on the treatment arm and the business model/patient management side of things. I love the collaboration with my physician colleagues, which is largely missing from the other disciplines within dentistry.
In summary, none of my studies, collaboration, or research would matter if it didn’t help patients. My advice is to find mentors, as I have, and trust the instincts we all have for good patient care. My role these days is to carry on what my mentors offered me and give the practicing dentist tools to help them be the best at improving the health of their community. Dental Sleep Practice Magazine will be a way for you to read about, and hopefully publish the great ideas you come up with.
- www.thumbsuckingbook.com
- “Phylogeny and Animal Models, an Uninhibited Survey” Chapter 5, Obstructive Sleep Apnea: Pathophysiology, Comorbidities and Consequences, Volume 3. 2008
- The Mandibular Repositioning Device: Role In The Treatment Of Obstructive Sleep Apnea. Stuart J. Menn, *Daniel I. Loube, Todd D. Morgan, Merrill M. Mitler, Joel S. Berger and Milton K. Erman. Division of Sleep Disorders, Scripps Clinic and Research Foundation, La Jolla, California, U.S.A.; and *Pulmonary Service, Walter Reed Army Medical Center, Washington, D.C., U.S.A.
- Initial Evaluation of a Titration Appliance for Temporary Treatment of Obstructive Sleep Apnea. Levendowski, DJ, Morgan T, Westbrook, P, J Sleep Disordered Therapy, 2011, 1:1 DOI10.4172
- Didgeridoo playing as alternative treatment for obstructive sleep apnoea syndrome: randomised controlled trial. Puhan MA1, Suarez A, Lo Cascio C, Zahn A, Heitz M, Braendli O BMJ. 2006 Feb 4;332(7536):266-70.
- Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009 May 15;179(10):962-6. Guimarães KC1, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G
- www.ptappliance.com