Dr. Michael A. Grandner discusses the Sleep Reset program that combines personalized coaching, education, and tracking components to promote healthier sleep habits.
 by Dr. Michael A. Grandner
by Dr. Michael A. Grandner
Poor sleep health affects a significant portion of the American population, with prevalent sleep-related issues impacting overall quality of life. A tiered approach to sleep health services is necessary, ranging from intensive interventions for severe issues to more widely accessible options for milder problems. Sleep coaching programs have emerged as a potential solution for addressing minor sleep concerns, offering education, support, and motivation to promote beneficial sleep habits.
While clinical interventions like Cognitive Behavioral Therapy for Insomnia are well-established for severe sleep problems, less-intensive interventions for subclinical issues are still limited. Sleep coaching interventions aim to bridge this gap by providing support for improving sleep behaviors. Some recent pilot studies have demonstrated the efficacy of sleep coaching in enhancing sleep health for various populations, including shift workers, military personnel, and adolescents with chronic illnesses.
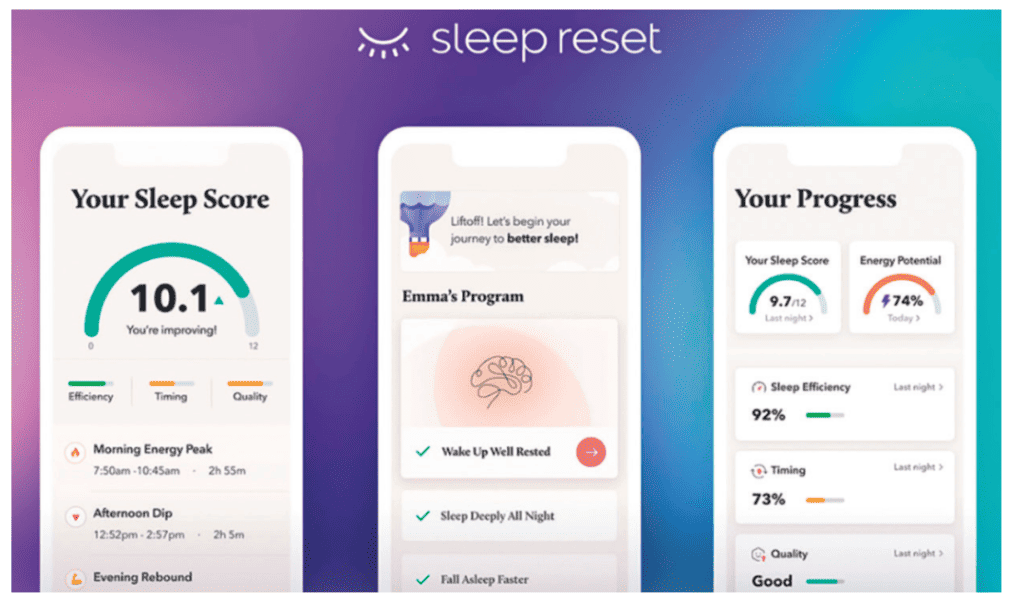
A recent study published in the journal Frontiers in Sleep evaluated the impact of a 12-week app-based sleep coaching program, called “Sleep Reset,” in a real-world setting. The program combines personalized coaching, education, and tracking components to promote healthier sleep habits. A total of 564 participants who completed the program were included in the study. They were initially screened for medical and psychological conditions that might contraindicate participation. Those individuals who likely needed more intensive care were referred toward clinical resources.
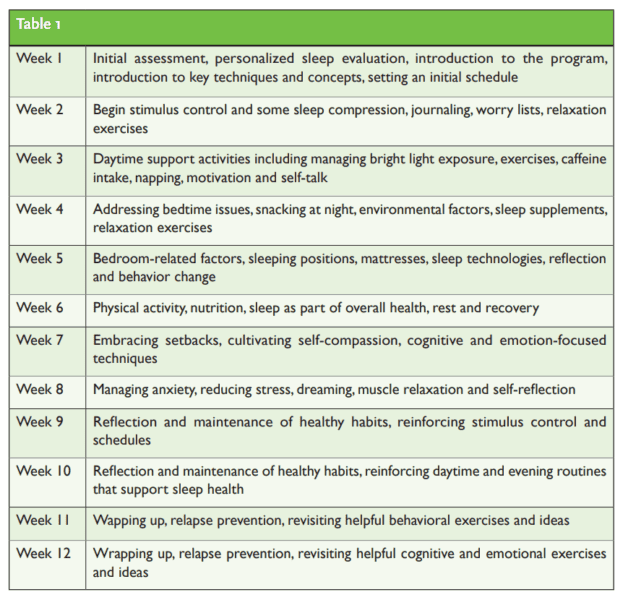
The Sleep Reset program spans 12 weeks and includes three main aspects: tracking and assessment, education on sleep and circadian habits, and interactive coaching with a live coach. The coaches communicate with participants through the app, offering personalized recommendations and feedback. The curriculum covers a range of sleep-related topics, from sleep compression to managing stress and anxiety (Table 1).
The study’s primary goal was to assess whether participants completing the Sleep Reset program would show improvements in sleep continuity (parameters like sleep latency, wake after sleep onset, number of awakenings, sleep efficiency), sleep duration, and use of sleep aids. It was hypothesized that participants would experience reduced sleep latency, wake after sleep onset, and awakenings, along with increased sleep duration and efficiency.
“Those who completed the Sleep Reset program on average saw notable, significant improvements in several dimensions of their sleep health.”
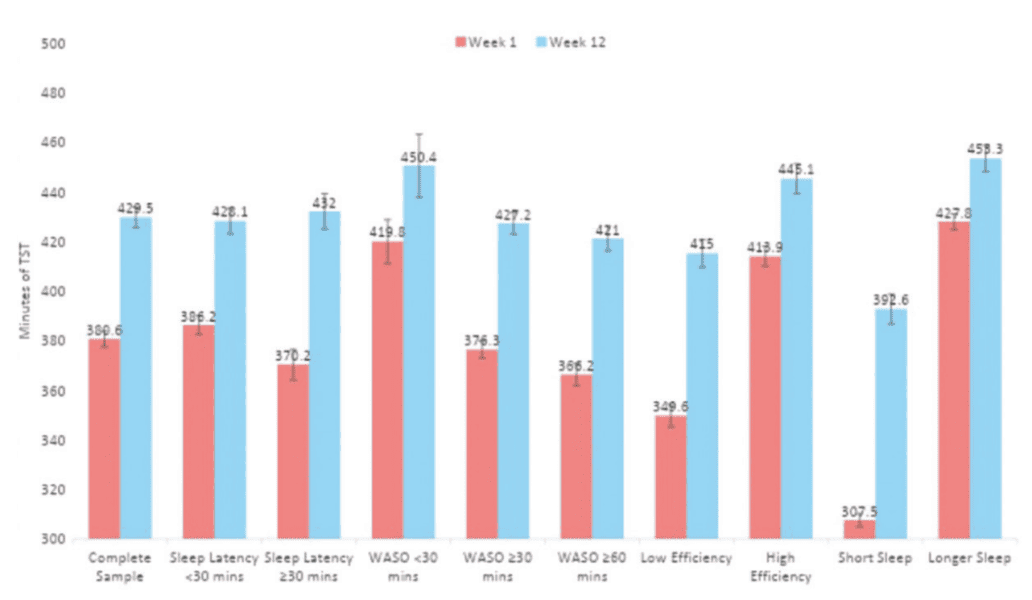
The results of the study demonstrated significant improvements in sleep parameters among participants who completed the program. Notably, there were reductions in sleep latency and wake after sleep onset, as well as improvements in sleep efficiency, number of awakenings, and total sleep time. Moreover, individuals with lower initial sleep efficiency and shorter sleep duration experienced more pronounced improvements. These findings suggest that the Sleep Reset program had a positive impact on sleep continuity and duration.
Among those who completed the program, they reduced their sleep latency by 41%, reduced their wake time after sleep onset by 35%, reduced their number of awakenings by 17%, increased sleep efficiency by a relative 8%, and increased sleep duration by about 45 minutes, or 11% (Table 2).

Like any sleep intervention, those who stand the most to benefit are more likely to see greater improvements. When those who started out with a lower sleep efficiency (<85%) were compared to those with a higher sleep efficiency at the outset, those whose sleep started out worse experienced greater improvements (Table 3).

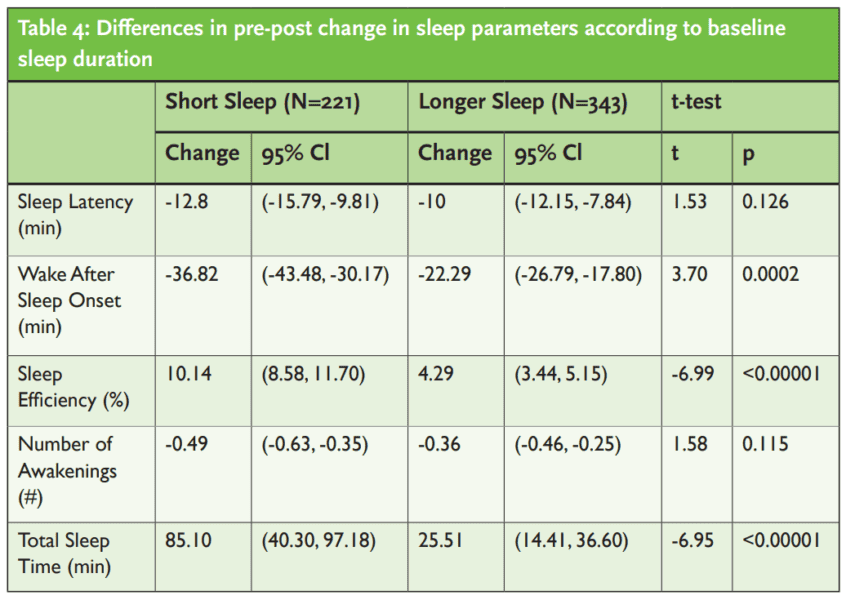
And those who started out sleeping less gained more sleep and improved their sleep to a greater degree than those who were already sleeping more hours (Table 4).
Taken together, those who completed the Sleep Reset program on average saw notable, significant improvements in several dimensions of their sleep health. They were falling asleep faster, staying asleep longer, waking fewer times, and sleeping more hours. These effects were especially pronounced for those who started out with worse sleep health, since they had more room for improvement.
The study has some important limitations, including the absence of a control group and the focus on program completers, which might introduce biases. The reliance on self-reported sleep data through diaries could lack objectivity. Rigorous methodologies, such as control groups and intent-to-treat analyses, are needed for a more accurate assessment of the program’s effects.
This study highlights the potential of an app-based sleep coaching program, Sleep Reset, in improving sleep parameters and sleep continuity for individuals without diagnosed sleep disorders. The multifaceted approach of coaching, education, and tracking appears effective in promoting healthier sleep habits. However, further research involving control groups and broader samples is required to confirm the program’s efficacy. As sleep-related issues continue to affect public health, interventions like Sleep Reset offer promise for enhancing sleep health in various populations.
Editor’s note: This article was adapted from Gorovoy SB, Campbell RL, Fox RS and Grandner MA (2023) App-supported sleep coaching: implications for sleep duration and sleep quality. Front. Sleep 2:1156844. doi: 10.3389/frsle.2023.1156844 and the complete article can be accessed here: https://www.frontiersin.org/articles/10.3389/frsle.2023.1156844/full
After reading about the Sleep Reset program, check out the stages of the sleep cycle and how to get a better night’s sleep in Dr. Lee Surkin’s article, “Sleep Stages and How to Improve Sleep Quality” at https://dentalsleeppractice.com/sleep-stages-and-how-to-improve-sleep-quality/


 Dr. Michael Grandner is a licensed clinical psychologist, board-certified in Behavioral Sleep Medicine and Lead Scientific advisor to Sleep Reset. He is the Director of the Sleep and Health Research Program at the University of Arizona and Director of the Behavioral Sleep Medicine Program at the Banner-University Medical Center in Tucson. Dr. Grandner is Associate Professor of Psychiatry, Psychology, Medicine, Nutritional Sciences, and Clinical Translational Science at the University of Arizona. He is an internationally-recognized expert in sleep health, has over 250 academic publications, and frequently consults with health, technology, athletics, and nutritional companies and organizations regarding sleep, health, and performance. Read more about him at
Dr. Michael Grandner is a licensed clinical psychologist, board-certified in Behavioral Sleep Medicine and Lead Scientific advisor to Sleep Reset. He is the Director of the Sleep and Health Research Program at the University of Arizona and Director of the Behavioral Sleep Medicine Program at the Banner-University Medical Center in Tucson. Dr. Grandner is Associate Professor of Psychiatry, Psychology, Medicine, Nutritional Sciences, and Clinical Translational Science at the University of Arizona. He is an internationally-recognized expert in sleep health, has over 250 academic publications, and frequently consults with health, technology, athletics, and nutritional companies and organizations regarding sleep, health, and performance. Read more about him at