iDentifySleep™ Training Series:
Sleep Disordered Breathing (SDB) Basics
An interview with Drs. Justin A Fu, MD, FAASM and Payam Ataii, DMD
Q. Why is snoring of interest to me and my patients?
Snoring may be disruptive to the quality of your patients’ sleep. Snoring may also be a sign of a serious medical problem.
 Q. What is snoring?
Q. What is snoring?
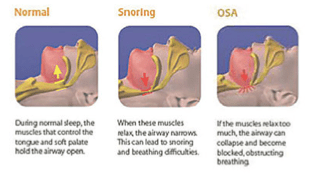
Snoring sounds are caused by airway tissues vibrating in response to narrowing of the airway during sleep breathing. These sounds are rarely troublesome to the snorer but may be to the bed partner.
Q. Why is snoring considered a sign of a serious medical problem?
Snoring may be a sign of sleep apnea, which results in poor sleep quality and can lead to excessive daytime sleepiness.
Being fatigued is a major cause of work-related accidents, car crashes, and loss of production.
Q. What is sleep apnea?
Sleep apnea is a potentially life-threatening condition that requires immediate medical attention. In fact, patients diagnosed with Obstructive Sleep Apnea (OSA) can’t breathe despite effort several times an hour for 10 seconds or more – sometimes, hundreds of times per night – preventing the brain and the rest of the body from getting sufficient oxygen.
 Q. How is sleep apnea categorized?
Q. How is sleep apnea categorized?
Sleep apnea is categorized in one of the following forms:
Obstructive Sleep Apnea (OSA): Is the more common of the two forms of sleep apnea. Generally, OSA is caused by a blockage of the airway, when the soft tissue and/or tongue collapse during sleep.
Central Sleep Apnea: As a result of instability in the respiratory control center, the brain does not signal the muscles to breathe, despite an open airway.
Q. Who is at risk for Obstructive Sleep Apnea?
Anyone at any age can have obstructive sleep apnea. Common risk factors for sleep apnea include:
 Large neck size
Large neck size
Large tonsils, a large tongue or a small jaw bone
High-vaulted upper arches
A family history of sleep apnea
Gastroesophageal reflux (GERD)
People whose bed partner has observed choking, gasping or loud snoring
Nasal obstruction (deviated septum, allergies or sinus problems)
Overweight or obese
History of Hypertension, Chronic Heart Failure or Chronic Obstructive Pulmonary Disease (COPD)
Q. What are the common signs and symptoms of Sleep Apnea?
Loud snoring
Choking or gasping during sleep
Fighting sleepiness during the day (even at work or while driving)
Morning headaches
Memory or learning problems
Feeling irritable
Inability to concentrate
Mood swings, personality changes, feelings of depression
Dry throat when waking up
Frequent night-time urination
 Q. What causes Sleep Apnea?
Q. What causes Sleep Apnea?
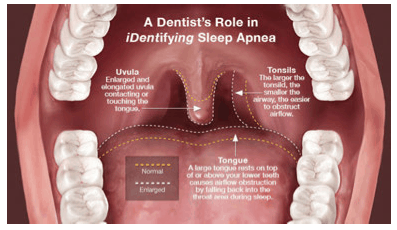
Under healthy airway conditions during sleep, muscles keep the throat open and tongue clear of the airway so that oxygen flows into the lungs. In Obstructive Sleep Apnea, however, the throat briefly collapses or the tongue blocks the airway causing a complete blockage of airflow. Along with those pauses in breathing, the oxygen level in blood may drop significantly.
Q. What is the Sleep Apnea prevalence?
Over 18 million Americans suffer from sleep apnea
An estimated 12 million Americans remain undiagnosed
Over 50% of all apnea cases are diagnosed in people aged 40 and over
Q. How is Sleep Apnea diagnosed?
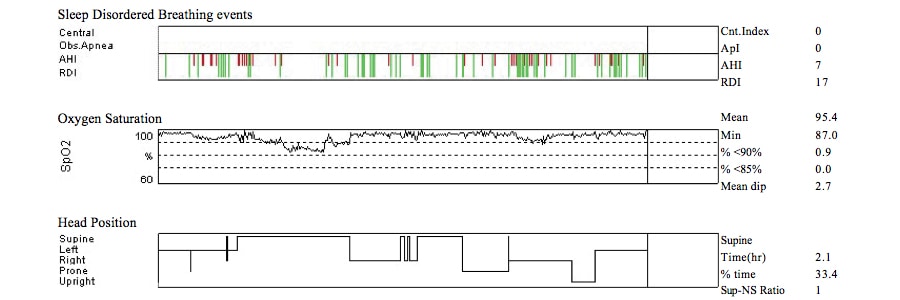
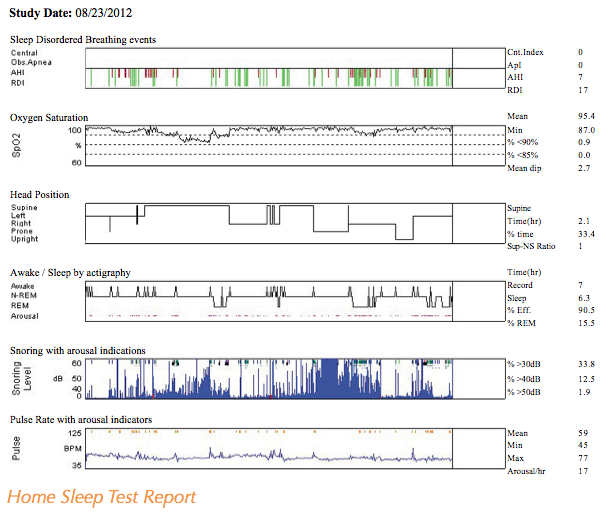
Sleep apnea is diagnosed by a properly trained sleep physician through the use of testing equipment designed to measure sleep breathing patterns. Testing may be performed at a sleep laboratory via a Polysomnogram or at the patient’s home using FDA-cleared ambulatory sleep testing equipment.
 Q. What is in Home Sleep Testing (HST)?
Q. What is in Home Sleep Testing (HST)?
A home sleep test is a simple-to-perform diagnostic procedure that patients can take in the comfort of their own home. While sleeping, the home sleep test device monitors the patient’s sleep patterns to include any pauses in their breathing. These FDA-cleared devices are designed to provide data for physicians to diagnose sleep breathing patterns.
 Q. What are the benefits of a Home Sleep Test (HST)?
Q. What are the benefits of a Home Sleep Test (HST)?
The patient self-administers the home sleep test, and is able to spend the night in his/her own bed in familiar surroundings.
Home sleep testing can be especially advantageous to the home-bound elderly who require specialized care such as a nurse or family member spending the night, expensive transportation costs, etc. HST is also beneficial for those with trouble arranging time out of their schedules to spend the night in a lab. The typical cost of a home sleep test is only a fraction of the cost of an in-lab sleep study, and yields effective results in the diagnosis of Obstructive Sleep Apnea.
Q. Why do over 10 million Americans with Sleep Apnea
remain undiagnosed?
Many sleep apnea patients remain undiagnosed because most often doctors are not properly trained on identifying patients with sleep apnea during a routine office visit.
Q. Are there enough doctors in America to treat sleep apnea?
Despite the fact that there is a growing awareness of sleep disorders and the number of persons that suffer from this condition is very prevalent, there aren’t enough physicians and dentists addressing this epidemic.
Q. How do dentists treat patients with sleep apnea?
Dentists may treat patients that suffer from sleep apnea through the use of FDA-cleared oral appliances. In fact, the American Academy of Sleep Medicine promotes the use of oral appliances as a viable option for patients that suffer from mild-to-moderate obstructive sleep apnea or severe patients when the patient cannot tolerate the use of a CPAP machine.
Oral appliance therapy involves the selection, fitting and use of a specially designed oral appliance that maintains an open, unobstructed airway in the throat when worn during sleep.
 Q. What is the Dentist’s role in identifying patients with Sleep Apnea?
Q. What is the Dentist’s role in identifying patients with Sleep Apnea?
Dentists may detect the less evident symptoms of sleep apnea through a candid conversation with their patients during an exam that addresses the patient’s concerns and dental health details. A dentist may suspect a patient suffers from sleep apnea if the patient complains about lethargy, morning headaches, or dry mouth (typically caused by open mouth breathing during sleep or heavy snoring).
If the patient shows enough risk of suffering from a sleeping disorder, dentists may prescribe a sleep study for the patient to rule out the condition.It should be noted that dentists are often the first professional to become aware of a potential problem since they are usually in contact with their patients more frequently than physicians.
 Q. How do I learn more?
Q. How do I learn more?
Give yourself 45 minutes and find out how to “DEMYSTIFY DENTAL SLEEP
MEDICINE” – A FREE WEBINAR SERIES PRESENTED BY Ez SLEEP
Register for a free, 1 CE Credit, 45 minute webinar:
Online: www.ezsleeptest.com/pillowtalk
Email: webseries@ezsleeptest.com
Phone: (888) 240-7735
Instructions on how to receive your CE Credit will be provided during the live webinar session.