When it’s time for appliance selection, it’s important to take into consideration patients’ physical needs and preferences as well as retention, allergies, and TMJ problems. Read about these considerations and more in this article by Dr. Jamison Spencer.
 by Jamison Spencer, DDS, MS
by Jamison Spencer, DDS, MS
Surgeons don’t get reimbursed based on the cost of their scalpel blades and sutures.
But that’s what dental sleep medicine providers are paid for – for the appliance – for giving someone a piece of plastic. We are NOT paid for our skills or expertise. As “Durable Medical Equipment” providers, we dispense durable medical equipment under an Rx from an MD.
The problem with how dentists are compensated in the U.S. and many other countries is that insurance companies pay for delivery of an appliance; a piece of plastic, acrylic, or nylon that has been cleared by the FDA because it looks like other appliances that have been previously cleared. Treating patients with sleep disordered breathing issues involves far more than the appliances we select.
The ongoing pandemic has even been cited as justification for mailing the pieces of plastic directly to patients for them to deliver themselves. There are certainly instances where this is indicated, appropriate, and medically necessary. However, there are already myriad reports of unscrupulous groups taking advantage of this limited use loophole to bill for “delivery” of the oral appliance, without providing any pre/post-care.
Get prepared now for the launch of oral appliance therapy “direct to consumer” campaigns. If a patient is deemed capable of handling their own orthodontic care, I assume there will be those investors who will believe such consumers are qualified to handle their own oral appliance therapy as well.
I blame the insurance companies and Medicare for this. They have set up the system, and we are trying to work within it. Why do we even try to work within their system? Because we’re trying to help as many people as we can, and for many of our patients, insurance or Medicare coverage is important.
While we continue to toil to get insurance companies to understand the immense benefit our experience, education, and expertise can provide patients via oral appliance therapy, we do need to ensure that we’re delivering oral appliances that are best indicated for each patient presentation. I’ll step off the soapbox and use it as a lectern.
In the Spring 2020 issue of Dental Sleep Practice, I wrote an article titled “The 3 Most Common Mistakes with Oral Appliance Selection.” I encourage you to revisit that article and check it out, but here’s a quick overview.
The 3 most common mistakes discussed were:
- Choosing an appliance that does NOT allow adequate lateral movement for a patient with evidence of historical lateral bruxism.
- Selling the appliance that you think will be the hardest for the patient to break.
- Falling victim to the “n of 1 syn”
As a continuation of that article, I’ve been asked to write a little more about appliance selection, and in this issue, I’ll delve into some of the less common, yet incredibly important, considerations.
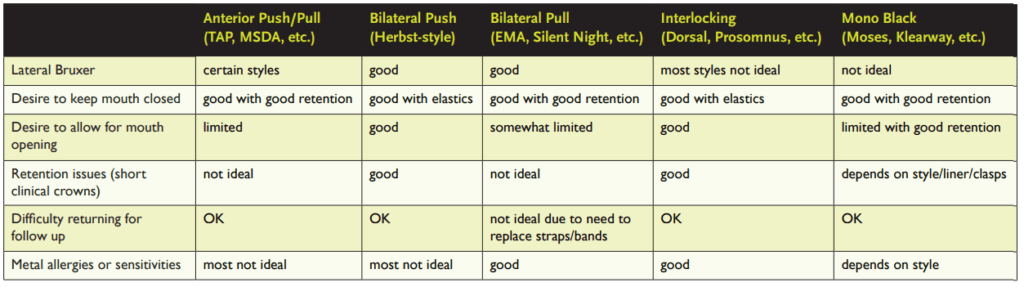
I segment the numerous appliances into 5 groups based upon mechanism of action. Those groups include:
- Anterior Pull/Push (TAP, MDSA, etc.)
- Bilateral Push (Herbst-style)
- Bilateral Pull (EMA, Silent Nite, etc.)
- Interlocking (Dorsal, ProSomnus, etc.)
- Mono Block (Moses, Klearway, etc.)
In general, certain types of mechanisms are better or worse for certain types of issues. Let me group some of the considerations into a few categories, and then briefly discuss each:
- Retention
- Patient preferences and convenience
- Prior experience
- Metal “allergy”
- TMJ problem
Retention
Retention related issues typically involve poor retention due to missing teeth and/or short clinical crowns.
When poor retention is likely, it’s better to choose an appliance whose upper and lower components aren’t connected, such as an interlocking style appliance (an appliance with “fins” of some sort), or a push style appliance (such as a Herbst). Often dentists will look at a Herbst-style appliance and think that when the patient opens wide it would dislodge, but there is virtually no resistance to opening with a Herbst (unless elastics are used) and the patient would have to open really wide before the pistons will lock out, which rarely occurs.
Patient preference and convenience
Under this category are things like the patient’s desire to be able to open their mouth fully because they’ll feel claustrophobic if they can’t, or technically merinthophobic – fear of being bound (thank you Dr. Rob Rogers for teaching me that). Other patients want the appliance to prevent mouth opening as they’ve found this was the problem in the past (particularly as they tried to use their CPAP). The anterior pull/push style is a great choice for patients who want to keep their mouth closed, but other appliance designs may also be used with the addition of vertical elastics. For the patient who desires the ability to easily open their mouth an anterior pull/push style is not the best choice.
Some patients may have a harder time coming in for follow-up due to distance of travel, transportation, or mobility issues. For such patients it may be prudent to provide an appliance that doesn’t require as much in-person follow up or exchanging of parts. For example, a pull appliance may be suboptimal because of the need to replace bands/straps. This can be done via mail if necessary.
The patient’s manual dexterity and vision must also be taken into account, particularly if they will not be able to easily come in for calibration of the appliance. It’s easier to adjust the position on some appliances than others. Additionally, some appliance designs make them readily adjustable via a phone call or telemedicine visit. If the patient can’t adjust the appliance themselves, perhaps they have a family member or caregiver who can help them.
Another consideration is future restorative dental care. Dentist #1 recently told me about a patient who was initially fit for a custom oral appliance by Dentist #2. Dentist #2 failed to contact Dentist #1, the patient’s dentist, in advance. The patient was already treatment planned for multiple restorations, but none of this was taken into account by Dentist #2 who fit the oral appliance. Neither the patient nor Dentist #1 were happy about this. It is usually not that difficult to plan ahead for pending restorative dentistry and to choose an appliance that may be easily modified or relined. You might even consider beginning with a temporary appliance when this situation arises.
Prior experience
I had a patient who’d previously been given a Herbst-style appliance. She hated it. And she’d tell you all about it. After getting to know her better and asking her a lot of questions, I realized that she didn’t despise the appliance. She deplored the dentist that gave it to her, and she had an overall negative experience at their practice. It really wasn’t the appliance. Still when I decided on the appliance to use in her case, I did NOT go with what she had been given in the past since she connected negative emotions with it.
Another time a physician came to me. She had been given a boil and bite snore guard (literally the “Snore Guard” – which is a specific branded appliance) by her general dentist a year prior. Her dentist referred her to me to take over her care. I figured that no self-respecting dental sleep medicine expert could possibly use such a “crappy appliance,” so I guided her into custom-fabricated one. Guess what? She hated it! I ended up making her another Snore Guard and have made her several more over the years.
I’m my experience, if a patient loves a certain appliance and they’d like a new one – just make it for them. They’ve become accustomed to it. They wear it. Isn’t that the goal?
Metal “Allergy”
This one is pretty obvious but frequently missed until it’s too late. Discuss any metal “allergies” with the patient if you’re thinking of using an appliance with metal. Why the quotation marks, my proofreading DSM gurus? Because many people who think they are allergic to metal aren’t actually allergic. HOWEVER, it’s not worth the battle to try to convince them otherwise, so I would rather choose an appliance that is metal-free.
TMJ Problem
This one isn’t actually about the appliance but is more about your skill and expertise as a clinician. It’s about diagnosing what their “TMJ problem” really is. What will be required to treat it, if treatment is indicated at all? Did they previously have a problem, but they haven’t for years? Do they have an internal derangement, such as a reducing or non-reducing disc displacement? Do you know how to tell? Could their relatively mild problem get worse? Could their relatively severe problem get better with oral appliance therapy?
Treating a patient with an existing or past TMJ problem is more about you than the appliance, however, depending on the diagnosis, there are certain appliance designs that would make more sense than others.
That’s a topic for another article. Use these guidelines. Talk to your patients, their other providers and think critically.
Read more about appliance selection in “Eeny Meeny Miny Moe: Selecting an Appropriate Appliance for Your Patients” here: https://dentalsleeppractice.com/articles/eeny-meeny-miny-moe-selecting-an-appropriate-appliance-for-your-patients/
 Dr. Jamison Spencer is the director of the Centers for Sleep Apnea and TMJ in Boise, Idaho and Salt Lake City, Utah. He is an invited lecturer on the topics of dental sleep and TMD around the world. His “Spencer Study Club” is the premier, members only, education and mentoring forum for smart and ethical dentists looking to implement sleep and TMD in their practices effectively and profitably. For more practical and often irreverent information check out his podcast, “The Airway, Sleep & TMD Podcast.”
Dr. Jamison Spencer is the director of the Centers for Sleep Apnea and TMJ in Boise, Idaho and Salt Lake City, Utah. He is an invited lecturer on the topics of dental sleep and TMD around the world. His “Spencer Study Club” is the premier, members only, education and mentoring forum for smart and ethical dentists looking to implement sleep and TMD in their practices effectively and profitably. For more practical and often irreverent information check out his podcast, “The Airway, Sleep & TMD Podcast.”