Help your ROI with technology
 Everywhere you turn dentistry is going digital. Now even dental sleep medicine is going digital! This is just the beginning, but the fact that digital dentistry is placing its mark on OSA therapy gives me great confidence in the growth potential of dental sleep medicine.
Everywhere you turn dentistry is going digital. Now even dental sleep medicine is going digital! This is just the beginning, but the fact that digital dentistry is placing its mark on OSA therapy gives me great confidence in the growth potential of dental sleep medicine.
Let’s take a look at a few areas where digital dentistry makes OSA therapy more efficient, predictable, and profitable. The beauty of this digitization is that it is not exclusive to just sleep therapy.
This is technology that you are or could already be using for many different areas within your practice – diagnostics, implant planning, orthodontic planning, and restorative dentistry. Now it has the ability to add dental sleep medicine to the mix.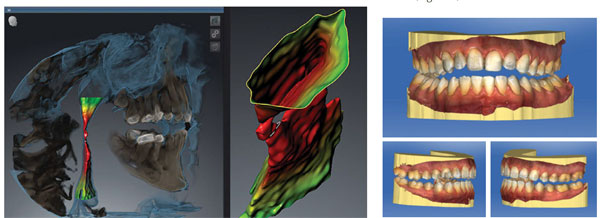
Creating Patient Awareness
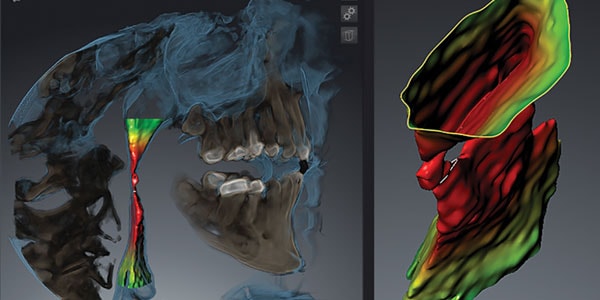
It’s great to work with the low hanging fruit of CPAP failures, but the real growth in your OSA practice comes when you can help get the roughly 80% of undiagnosed sufferers on their way to healthier sleep breathing. To do this you must find a way to create awareness and urgency in those unaware. For me this is best done by utilizing 3D CBCT imaging (Figure 1).
While NOT diagnostic for OSA, it certainly creates an avenue to having a conversation and encouraging your patient to have either an HST (Home Sleep Test) or in lab PSG.
Since implementing airway segmentation into regular hygiene recare visits and new patient visits we have seen an increase of unaware patients entering into our OSA therapy workflow.
Reducing Chairtime
Digitization also helps increase your profitability by reducing chair time. Nothing is more expensive in your practice than your chair time. Adjustments and remakes can wreak havoc on your profitability and not to mention patient confidence.
The fit of your OSA appliance is an important part of patient comfort, compliance, and effectiveness. Too often we spend time adjusting appliances due to poor quality impressions and general inaccuracies of analog fabrication methods. We can now leverage digital impressions to produce appliances that are more accurate and minimize adjustments (Figure 2).
Another unrealized benefit of digital impressions is faster turnaround time. It is often hypocritical of me to tell the patient the importance and urgency of getting into an appliance and in the same breath tell them it will take several weeks for the lab to make the appliance. Digitization has allowed us to get appliances back in about a week
(Figure 3).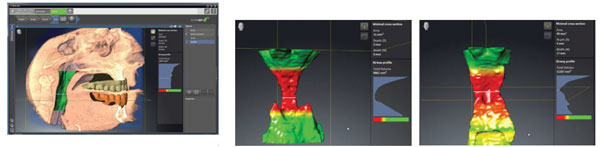
The Bigger and Complete Picture
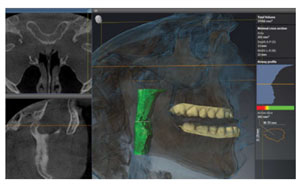
Dental sleep medicine is truly an area where we can begin to help patients with overall health improvement. As with any health therapy there are potential complications and/or side effects. 3D imaging gives us an opportunity to evaluate many of these areas prior to commencing therapy.
One area that has long been a concern for OAT has been its potential affect on the joint. While there are many reasons for this, most commonly it’s due to undiagnosed joint issues prior to treatment or an inappropriate bite putting the joints in an uncomfortable position. 3D imaging allows you to visualize the joint pre-treatment and avoid potential issues (Figure 4).
Being able to evaluate the joint is a worthwhile benefit of 3D imaging. At the same time we can also measure potential airway change. Using the same 3D image we can also measure the airway with the bite and/or appliance in place. Personally, I prefer to take it with the bite in place. This allows me to compare the potential airway changes prior to having the appliance fabricated (Figure 5).
Please don’t misunderstand me. A post treatment HST or PSG is the ideal and standard measure of treatment effectiveness.
Having the ability to measure airway, evaluate joint position, and see anatomical deviations gives me a more complete picture of airway therapy. This leads to more predictable results and better communication between dentist, physician, and patient.
Digital dentistry has made restorative and implant dentistry more predictable, efficient, and improved clinical outcomes. It is poised to do the same for oral appliance therapy. This is just the beginning and it’s exciting to see what is in store for the future.
 Dr. Tarun Agarwal is a nationally recognized lecturer in the field of aesthetic and restorative dentistry. He practices in Raleigh, NC. In July 2002, he co-founded the Dentaltown “Townie Meeting” an annual event considered one of the most progressive educational opportunities in dental education. Dr. Agarwal has assisted numerous dental manufacturers in new product development and review. He has been featured on ABC, NBC and CBS news and several consumer magazines for his pioneering use of technology, philanthropic events, and aesthetic dentistry. In 2003, Dr. Agarwal was voted the “Townie of the Year” for his contributions to the growth and dynamics of the dental community.
Dr. Tarun Agarwal is a nationally recognized lecturer in the field of aesthetic and restorative dentistry. He practices in Raleigh, NC. In July 2002, he co-founded the Dentaltown “Townie Meeting” an annual event considered one of the most progressive educational opportunities in dental education. Dr. Agarwal has assisted numerous dental manufacturers in new product development and review. He has been featured on ABC, NBC and CBS news and several consumer magazines for his pioneering use of technology, philanthropic events, and aesthetic dentistry. In 2003, Dr. Agarwal was voted the “Townie of the Year” for his contributions to the growth and dynamics of the dental community.

