by Joy L. Moeller, BS, RDH
Many dental offices are involved in the treatment of sleep disorders, restricted frenums, orthodontics, cosmetic dentistry, oral facial pain and pediatric dentistry. New studies are now validating the collaboration of the treatment of myofunctional disorders as an adjunctive protocol for obstructive sleep apnea. Sleep specialists are now being taught about the value of working with myofunctional therapists for more comfort with CPAP and MAD.1 Because dental hygienists see their patients for recall visits on a regular basis, a screening for myofunctional disorders should be performed and recommendations for therapeutic treatment should be made which can be part of the services offered in a dental office.
Most successful dental practices have busy hygiene programs and many wonder, “How can I build myofunctional therapy into my practice, retain my patients seen for regular hygiene services, and provide more comprehensive care?” A sizable segment of hygienists have either carpal tunnel, burn out, or shoulder issues and are in search of new pathways to provide new services that are interesting, challenging, and bring value to the patients and the practice. After taking a course and extensive internship, I began seeing patients after work or on my day off and the dentist I worked with was happy to have his patients cared for. I remunerated him based on a percentage of collections, used my own phone, bought my own supplies, bought my own insurance, made my own appointments, and made sure the office was left clean and neat for the next day. He treated me as a colleague or associate and I felt respected and valued.

Benefits for the office include:
- Referrals from other medical and dental providers; Frequently these referrals become new patients of record
- Happy patients referring new patients
- Residual income for the office
- Adjunctive treatment was geared to enhance and improve services already offered in the practice such as TMD2, Orthodontics, Sleep Dentistry, Periodontal Therapy, Pediatrics, etc.
- I provided marketing of my services though lunch and learns to possible referral sources, wrote articles in our local papers, and attended meetings which built our name in the community.
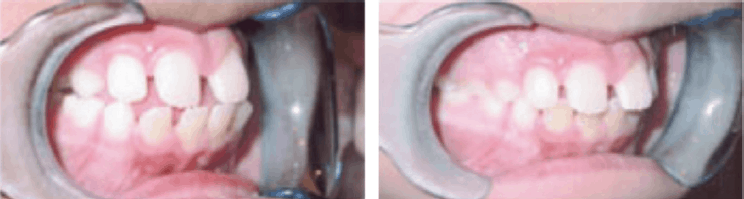
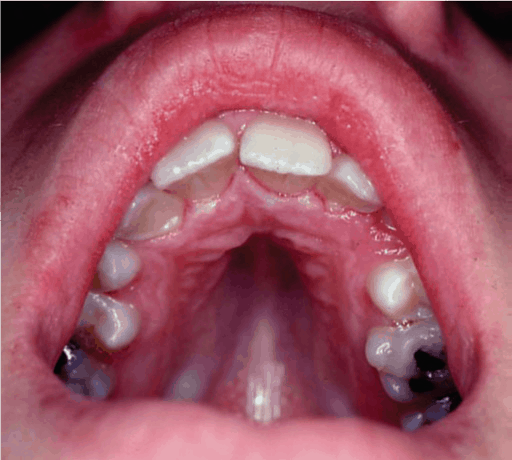
What is involved in developing a program for the treatment of myofunctional disorders? First, the patient and the practitioner must become aware of these disorders and their impact of not only oral health, but systemic health as well. Research articles, before and after photographs, and intra-oral cameras to show the patient what is happening in their mouth are important tools. The Mallampati, Friedman score, Epworth Sleepiness Score, or other sleep screening, observing the patient swallowing, breathing and chewing are all tools that can be utilized to determine need for a more in-depth evaluation.


Myofunctional therapy has been known in the orthodontic field since the early 1900’s.3 Approximately 10 years ago, I was called to Stanford University to lecture for the Sleep Department on myofunctional therapy and sleep disorders by Professor Christian Guilleminault. After following the Brazilian studies,4 that meeting influenced Stanford University to begin doing research to prove that myofunctional therapy, breathing education, and frenum restriction release may assist in the treatment and prevention of obstructive sleep apnea.5
The next question becomes who, amongst current health care professionals in the USA, has it in their scope of practice to take on the responsibility of the treatment of these disorders? The American Dental Hygienist Association has had it in their position statement for dental hygienists since 1992.6 Also, speech language pathologists, occupational therapists, physical therapists, and nurse practitioners may also be qualified to treat patients with myofunctional disorders with post-graduate training.
What does this mean for hygienists? We now have agency to utilize all those anatomy, physiology, psychology, pharmacology, and pathology courses that we had to learn. We are the principal dental health educator in the office, and we can be proactive with children to eliminate noxious habits and improve nasal breathing, lip seal, chewing, swallowing and proper tongue rest position. As far as periodontal disease, we have known for many, many years that mouth breathing can cause inflammation of gingival tissues but we never treated the functional breathing of our patients.7
Because dental hygienists have had training in proper nutrition, we now can add the functional aspects of proper selection of whole foods and why and how to properly masticate and swallow the food correctly. In doing this, the myofunctional disorders may be more successfully treated and eliminated.
The tongue is comprised of 16 different muscles that have different functions of moving the food in the mouth, developing a bolus which is safe to swallow without choking,8 and maintaining proper airway with the back or base of the tongue. If the frenum is restricted, the posterior airway may be compromised contributing to sleep apnea.9

Dental hygienists have training in psychology and motivation. Much of the success of myofunctional therapy depends on patient compliance at home and with subsequent appointments (either in person or with tele-practice). For pediatric patients, we must enlist the parent in supporting the treatment. Parents must understand the value of how myofunctional therapy may avoid learning disabilities and reduce behavior problems with proper oral postures. This is in the dental hygienists’ wheelhouse.
Because myofunctional therapy relies on active patient participation, we must use several techniques that are based on the ten principles of neuroplasticity.9 Neuroplasticity means the ability of the brain to change, following physiologic or pathologic input, generating an adaptive response. We must look at and teach the possible cause of the problem in order to understand the treatment so that the patient will understand why therapy is necessary.
Therapy consists of sequential, therapeutic techniques, done over a period of three months and followed for at least one year until the patient has successfully habituated the new muscle patterns and functions. The important goals of myofunctional therapy are:
- Developing a lip seal
- Attaining palatal tongue rest position
- Awareness and elimination of oral habits
- Restoring nasal breathing during sleep, sport, and speech using the proper volume and rate of breathing
- Teaching bi-lateral tooth contact when swallowing and proper chewing and gathering foods in the mouth
- Establishing functional posture training, including sleep position


Some Benefits of Myofunctional Therapy
- Enhance orthodontic treatment (decreasing time and propensity for relapse)
- May correct problems with swallowing/digesting food (stomachaches from air swallowing)
- Can aid in functional speech impediments (lisps with saying “s” sounds)
- Helping ADHD though establishing proper breathing and tongue function
- May provide relief of TMJ dysfunction and teeth grinding by enhancing proper muscle functions
- Elimination of oral habits such as nail biting, thumb sucking, lip biting and licking
- Proper head and neck posture
- Reduction of gingival inflammation due to mouth breathing
- Snoring reduction or elimination, reduction of AHI, enhancing use of CPAP or OAT
- Improvement of facial esthetics by enhancing muscle functions such as lip seal and development of facial symmetry
Where can the dental hygienist be trained to become a myofunctional therapist? Currently in the United States, post-graduate courses are being taught through professional organizations such as the AOMT (Academy of Orofacial Myofunctional Therapy), independent practitioners, and some commercial entities. It is best to study more than a “weekend” course. In addition to the “basic” or “intro” course a serious, practitioner must incorporate a body of knowledge which includes breathing re-education, TMD, sleep, posture and frenulum restriction which are essential courses in order to become a qualified therapist.