I am a nice person. In fact I’m so nice that I told my front desk team members to always let sales reps through. My team doesn’t need to be a gate keeper because I’m always willing to at least meet them. I most likely will not buy from them, but hey, they’re just trying to make a living. I was known as the nice dentist to pay a visit to until the day a distributor representative came by. We are a very busy general dentistry PPO practice. We do all facets of dentistry including extractions and implant placement. My niche however is screening and treating sleep apnea. Dental Sleep Medicine has revolutionized my practice and my life. I love it. That day, the distributor representative was trying to sell me on cone beam. His angle? He was trying to sell me on cone beam’s use in DSM. I about became unglued. “There is no correlation to someone that is upright and awake to someone that is horizontal and sleeping!” He walked, almost ran, away as soon as possible and never brought it up or visited again.

Fast forward two years to the day I started teaching a Dental Sleep Medicine 101 course with Dr. Tarun Agarwal at his teaching center in Raleigh, NC. His courses center around 3D and digital dentistry workflow. Of which I had none. I told him from the start I would teach the sleep apnea, but I wouldn’t teach that a dentist should own a CBCT in order to treat sleep apnea. In fact, he could do all of the instruction in that area. I had every objection in the book and admittedly I was very closed-minded. As I already said, how could an upright awake airway give us an idea of what is happening at night? This shouldn’t even be used for screening. What if the patient happened to swallow during the scan? Why expose a patient to extra radiation? Why spend the extra money on a bigger field of view? Guess who is now a proud owner of both a CEREC and Orthophos SL with SICAT AIR? I saw how drastically this technology can benefit my patients. At first my business partner thought I was crazy. That’s a huge investment for a small town PPO practice, but we are already seeing returns.

Comparative airway view
I often get asked the best way to screen existing dental patients for potential OSA. Many offices have every patient fill out an Epworth Sleepiness Scale as a screener. Some offices measure necks. Some offices look at Mallampati. The problem with these techniques is that patients don’t make a connection and it’s one more thing for the team to do. The patients don’t see the value and rarely accept any ownership of a potential life-threatening disease. “I don’t have a problem with snoring, it’s my spouse that has a problem with my snoring.” You’ve all heard that before, right? A visual picture of their airway on a huge screen in front of their face opens their eyes and can start to connect the dots for the patient. The software is so easy to use that the team gets excited to incorporate this educational tool to their flow. The patients make a connection, they want more information, and they start the conversation. The awareness in my practice was already high but adding SiCAT Air airway images during an exam has elevated it that much more. The patients move forward.

Dr. Elliott preparing a patient for a scan using the ORTHOPHOS SL 3D
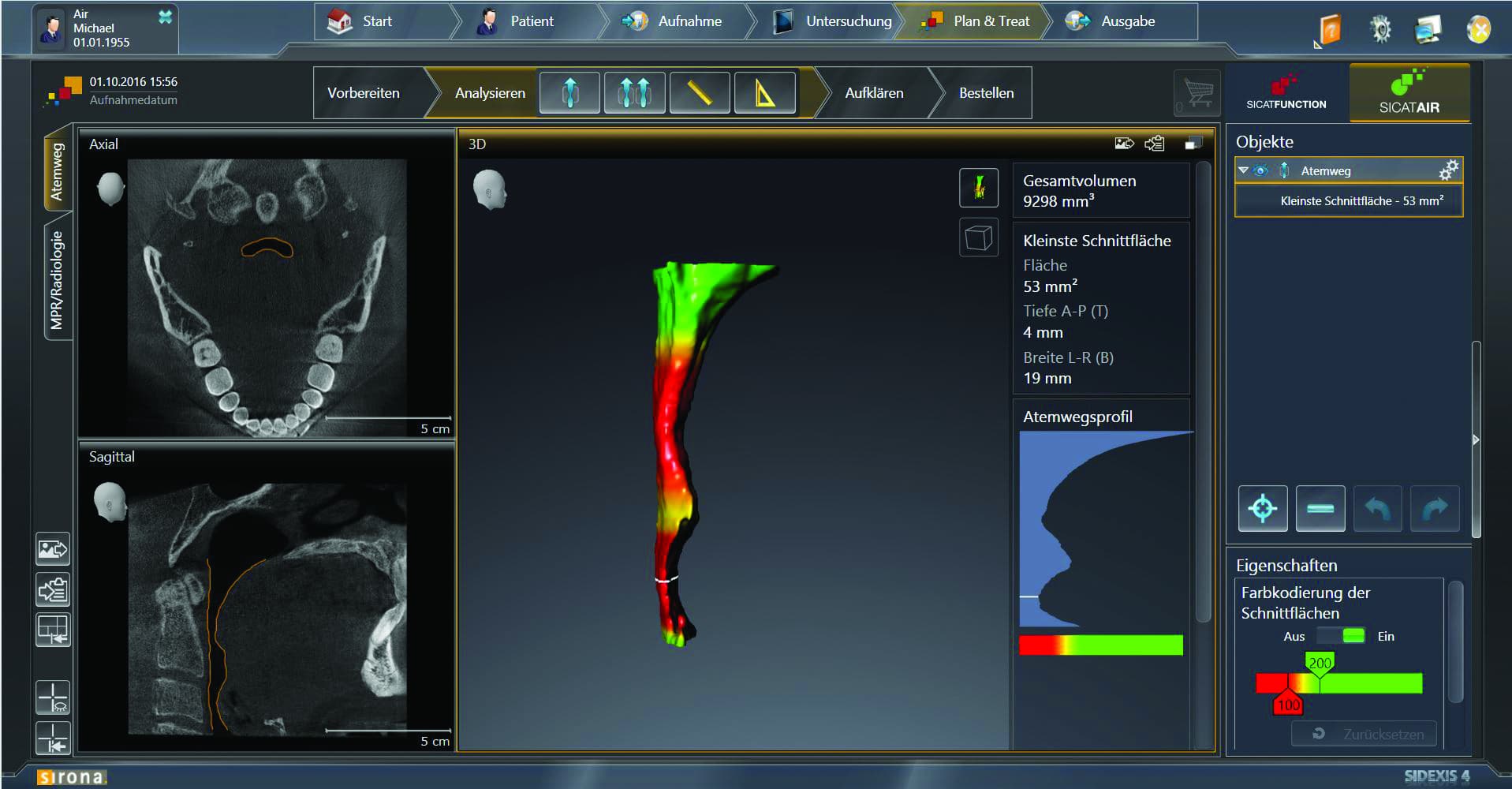
Airway before treatment with appliance
Each of my objections to utilizing 3D has slowly melted away. We take a 3D image on every new dental and sleep patient. As a general dentist office, the 3D image has helped us find restorative work we wouldn’t have found until the patient was symptomatic. We have found abscesses, resorptions, fractured roots, failing endo and helped plan predictable implants we might have referred out before. The patients are thankful and case acceptance has increased because the patients aren’t just being told what they need, they have participated in the discovery of it. Our practice is set apart. And guess what? The radiation is minimal. You could almost compare the exposure to radiation from a patient scan in my office to the flight I’m on right now, minimal.
In sleep, I get the advantage of having a baseline of the patients’ joints. In addition, I can get a better visualization of soft tissue that may compromise our treatment with an oral appliance. In the past I would do a visual exam of the nasal passage and evaluate the patient for nasal patency by having the patient breathe deeply through their nose. Now I can visualize their nasal passageways much more effectively. I can prepare the patient that the appliance alone may not fully treat their snoring and an ENT referral may be necessary. My dad always said that if you don’t prepare the patient beforehand and must explain it afterwards it just looks like you’re making excuses. I would rather the patient had realistic expectations in their treatment and I have better information.
Doug is a typical patient in our practice and happens to be a good family friend. He has been in our practice long enough that it was time to update his full mouth series. We did a scan, 4 bitewings and some anterior PA’s. First, we found external resorption on tooth #4. In the past, we would have seen something that looked suspicious on the PA, possibly send to the endodontist or wait and watch. The endodontist would have taken their own scan, deemed it hopeless, and then try to decide who was going to extract and place the implant. Phew… I’m tired and I’m not even the patient! Or we would have waited, “watch” it get bigger and have Doug call me on a Saturday in a ton of pain. We extracted the tooth at our office, immediately placed the implant and restored the tooth just last week. Doug is what we call a little bit of a “scaredy cat” but could not stop talking about how seamless and painless the process was. Even better is the conversation we had regarding his snoring.
His wife, Cindy, and I have been conspiring about his snoring for years but he was always in denial or never saw the perceived benefit. He was relatively young, fit, never tired and “slept just fine.” He had some sleepless nights because of stress at his job, not sleep apnea. That’s an “old person’s disease” he always said. But I also knew about his frequent visits to the urgent care for sinus infections and Cindy’s complaints of his snoring that made it impossible for her to sleep. By utilizing the tools that I was already using for dentistry, I could show him his obstructed nasal passageways, his thickened mucosal lining, and a volumetric scan of his narrowed airway.
Suddenly, the light bulb went off. He was finally willing to do a home sleep test that revealed moderate sleep apnea. He started to “own” that he had a problem and we created a sense of urgency. He even said, “I came in here trying to solve my snoring for my wife and now I realize I need to do this for my health.” With my new digital workflow, we could make this happen in less time than my traditional impression workflow as he was anxious to get help. I took a scan prior to a protrusive bite and then another with the bite in place. I imported his digital impressions into the SiCAT software and clicked “Order.” It was very simple. After ENT treatment and an appliance, Doug and Cindy both sleep more peacefully… and so do I knowing that I could lead one more person toward better health.

Optisleep
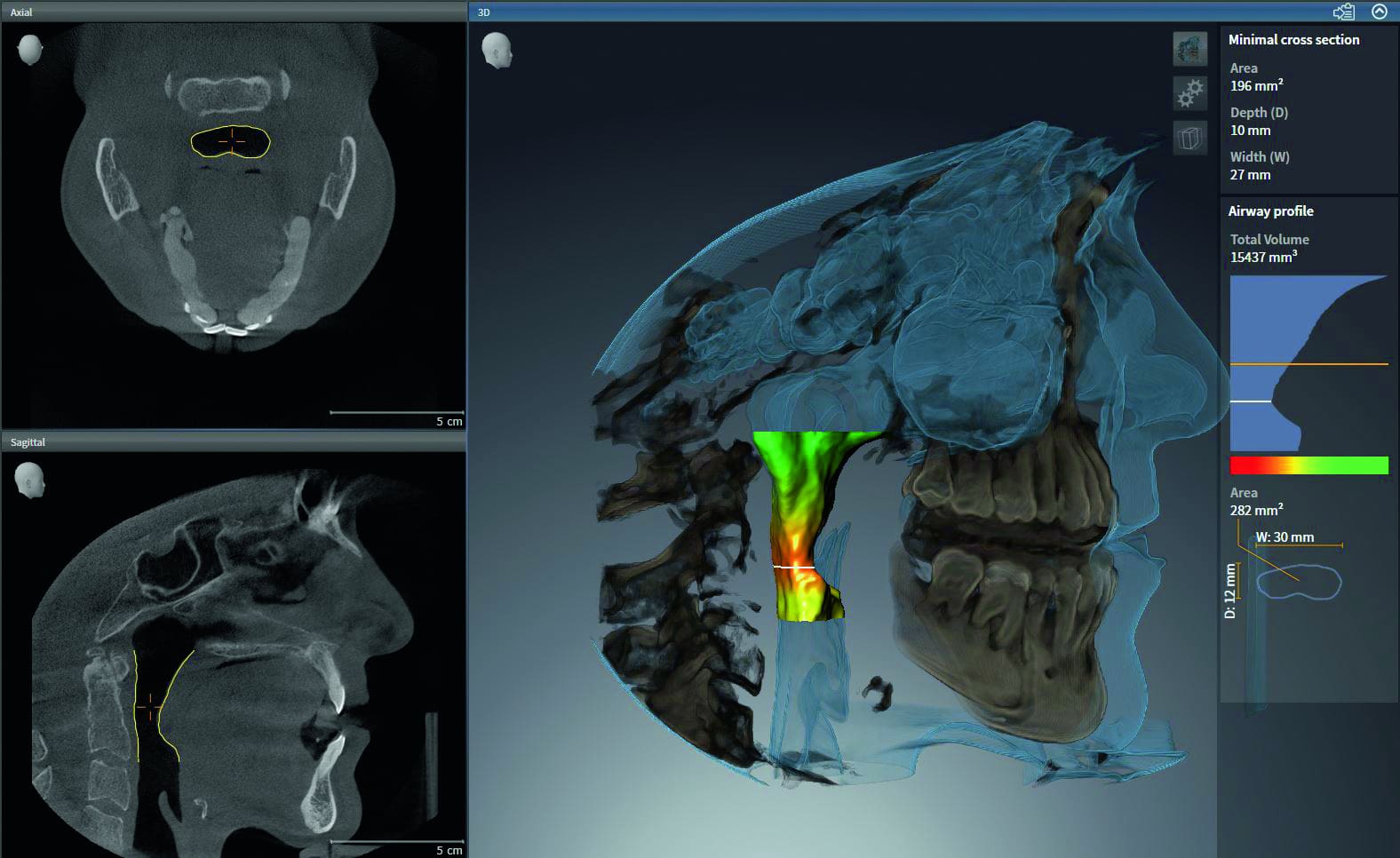
SICAT AIR screenshot showing airway volume
The distributor rep and I have long since made up, and he no longer tries to bypass me to talk to my business partner. Because of the investment we made in our practice, my patients feel the value we put on their health, and that makes me feel like a nice person once again.