CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims & objectives
Dental Sleep Practice subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will exhibit the reader will:
- Understand the difference between various subjective and objective screening modalities for sleep related breathing disorders
- Recognize the difference between traditional pulse oximetry and high resolution pulse oximetry
- Identify when and with which patients to use high resolution pulse oximetry to screen for sleep related breathing disorders
- Recognize important indicators on high resolution pulse oximetry reports in order to identify which patients are appropriate to recommend potential sleep therapies
Editor’s intro: Craig Pickerill discusses how high resolution oximetry can be a cost-effective and minimally invasive screening method for sleep-related breathing disorders.
by Craig Pickerill
Sleep related breathing disorders place a substantial monetary burden on the economy in the form of decreased productivity, work accidents, and health-related complications.1 Experts in dentistry, pre-surgical screening, cardiology, occupational health, and primary care find that their respective fields would benefit from screening, but polysomnography is often too expensive and impractical. However, recent technological advancements in high resolution pulse oximetry make it a straightforward, cost-effective tool, allowing more patients to be willingly evaluated.
Overnight pulse oximetry monitoring is also a cost effective and minimally invasive method for the dentist to adjust a dental device prior to a follow-up home sleep apnea test (HSAT) or facility-based polysomnography (PSG). While at least one follow-up HSAT or PSG is usually required, using oximetry reduces the likelihood that the patient will need to return for additional HSATs or PSGs.
Subjective vs. Objective Screening Tools
Overall, any health screener is used to indicate the next step – no treatment for those with no risk, more testing for people at high risk of having the disease being looked for. Screeners do not provide diagnosis – they are used to choose which people would benefit from increasingly sophisticated diagnostic tools.
There are many subjective patient screening questionnaires for sleep related breathing disorders (SRBD) currently in use in various professional settings. These include the American Society of Anesthesiologist’s Checklist, the Berlin Questionnaire, STOP-BANG, STOP, and the Erlangen Questionnaire. These questionnaires are generally easy for patients to use and are low cost.
However, the use of subjective questionnaires alone is problematic. The US Preventative Services Task Force found that validated questionnaires did not correctly identify who would benefit from sleep testing.2 They tend to have a high false positive rate, making patients and health care professionals believe everyone will screen positive. While some questionnaires have undergone rigorous validation, others have not been proven scientifically accurate. Also, there is no stratification of risk – all patients are shown to be at the same risk level, and they do not differentiate by cause of sleepiness, such as not getting enough sleep vs. SRBD. Finally, patients can falsely answer questions to match employment requirements, such as in the transportation industries. Because of the high false positive rate and other aforementioned factors, they poorly convert patients to get further testing and sleep therapy. For example, it was found in one study of Type II diabetics where only a screening questionnaire was used, while 90% were found to be at risk for sleep related breathing disorders, only 17% initiated therapy.2
Objective screenings can provide dentists with much more accurate and specific information when screening for SRBD. Physical exams, such as the Mallampati, can be utilized. The Mallampati test scores the distance from the tongue to the roof of the mouth into different classes; higher classes are associated with increased risk for SRBD.2 However, the original intended use of the Mallampati was to predict difficulty of intubation, and some research has found it less effective for screening SRBD.3
High Resolution Pulse Oximetry is an Increasingly Used Technology for Sleep Related Breathing Disorders Screening
Pulse oximetry is increasingly being used as a screening tool for several reasons. It works by passing red and infrared lights through the tissue in the finger and analyzes how much light was absorbed by the red blood cells. The amount of oxygen in the blood can be measured, giving an oxygen saturation reading.6 It is widely available, most insurance plans cover it, it is relatively simple for patients to utilize, painless, and it is inexpensive when compared to polysomnography or home sleep studies. Further, oximetry results have been shown to provide similar predictive results as that of home sleep studies4 as well has having both high sensitivity and specificity for sleep related breathing disorders.8
The Role of High Resolution Pulse Oximetry (HRPO) in Screening for Sleep Related Breathing Disorders: High Resolution Pulse Oximetry vs. Traditional Pulse Oximetry
The accuracy of the results for the screening of SRBD can be affected by the type of pulse oximeter that is used. Advancements in technology have led to pulse oximeters that utilize faster, more accurate sampling rates and sophisticated motion artifact algorithms. These advancements can detect more respiratory events and compensate for patient movement. This in turn helps identify patients that are at high risk of having obstructive sleep apnea.
When comparing pulse oximeters, the sampling rate, signal resolution and motion algorithms can help determine the accuracy of the results. Traditional oximeters use a sampling rate that can be 4 seconds or more. The signal resolution is rounded to the nearest 1% SpO2. “High resolution” in pulse oximetry typically refers to one or both of the following:
- Signal Resolution: Some HRPO’s include a signal resolution of 0.1% SpO2, which showed better detection of shorter apneas and improved reproducibility in 2010 comparison study.9
- Averaging Time: A shorter averaging time, or also known as weighted moving time, is important. This moving window averages data across time intervals during the test. Studies show that increasing the window length of an oximeter’s moving average causes underestimation of desaturation events. Although lengthening moving averages may artificially improve a pulse oximeter’s ability to hide unwanted noise, this may lead to the underestimation of the frequency of desaturation/resaturation events and extent of desaturations.9
- Sampling Rate: High Resolution pulse oximeters (HRPO) incorporate a sampling rate of >1 / second. Lower sampling rates can underestimate event amplitudes to apneas and miss events. This can cause an artificially low oxygen desaturation index (ODI).
High resolution pulse oximeters, such as Minolta 300i and SleepSat, have a signal resolution of 0.1% and short averaging times, resulting in higher sensitivity and sensitivity. A study showed sensitivity was improved from 0.81 to 0.97 vs polysomnography (PSG) when HRPO changes were made. It is important to note a higher sampling rate doesn’t improve sensitivity unless it has a high signal resolution also. The results of this study suggest that the new algorithm with improved response to apnea/hypopnea events and higher oxygen saturation resolution is superior to the old algorithm.11 Comparison of the HRPO results to meta-analysis of HSAT shows the oximeter’s sensitivity outperforms HSATs when compared with polysomnography in the lab.10
In summary, high resolution pulse oximetry will be best suited to detect minor sleep related breathing disorders if it includes both storage of SpO2 to the tenth (.1%), AND data stored at 1 Hz (once per second).
Understanding High Resolution Pulse Oximetry Results

After receiving the results of HRPO, it is important to understand the results for the patient’s next step of care. Oximetry, home sleep apnea tests, and PSG software applications will typically report the number of desaturations per hour, and time recorded in defined oxygen saturation ranges. Profox oximetry software, for example, works with several oximetry devices and provides this type of summary data. Other device manufacturers, such as Nonin with PureSAT technology, have improved this type of reporting by enhancing the oximeter’s ability to record accurately during movement or low perfusion. This leads to a more accurate representation of desaturations per hour, minimum and maximum SpO2 and time spent in oxygen saturation ranges. Lastly, some software providers take advantage of the data collected by HRPO devices to provide advanced reporting features. SatScreen oximetry reporting software, for example, has developed baseline drift and severity indices to better stratify the type and severity of sleep-disordered breathing.
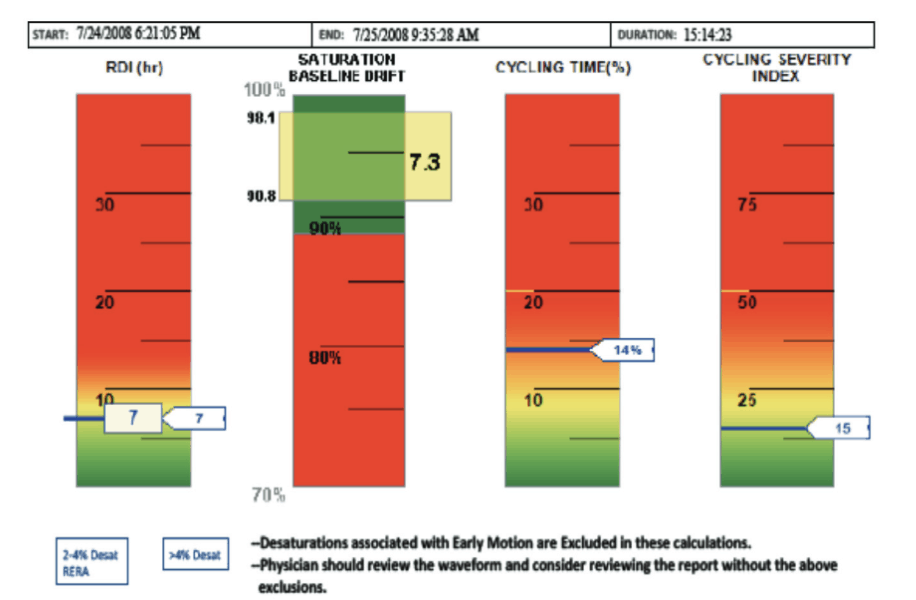
In Figure 2, the overnight results are summarized in a set of bar graphs where green areas represent normal values and red areas represent moderate to severe values. It is generally recommended to obtain 4 or more hours of data.
One of the indicators often used to screen for SRBD is the respiratory disturbance index (RDI). The RDI as defined herein as the average number of desaturations and respiratory effort related arousals (RERAs) per hour. A desaturation event is a breathing event with a 4% or more reduction in oxygen saturation. RERAs are events that are 10 seconds or more where upper airway resistance causes an arousal. It is adjusted for oximetry to represent mild desaturations with abrupt pulse rise and indicates the number of mild respiratory events which may be disruptive to sleep. In the example report above, the hourly index for minor desaturations associated with autonomic arousals is recorded on the left side of the bar graph. The hourly index of desaturations equal to or greater than 4% are recorded on the right side. The overall respiratory index is noted in the center. Normally, an RDI of 5-14 indicates risk of mild sleep apnea, 15-29 indicates risk of moderate sleep apnea, and 30 or more is at risk for severe apnea. A symptomatic patient who does not fulfill the diagnostic criteria for OSA might have Upper Airway Resistance Syndrome (UARS).12

The saturation baseline drift is an indicator for potential sleep hypoventilation. It is shown on the second bar graph with the highest baseline and the lowest baseline marked. This indicator represents the magnitude of decline from the highest to the lowest SPO2 baseline independent of acute respiratory events. A low baseline that falls in the red section of the indicator (≤88%) may be clinically significant.
While the number of desaturations per hour is key to determining apnea risk and severity, oximetry reports including cycling time and cycling severity may provide additional insight into the patient’s disease state. The cycling time indicator represents the percentage of the total study time the SPO2 exhibits a cycling pattern of ventilatory instability. The cycling severity Index accounts for depth of the desaturation events, the duration of the desaturations, and the recovery time between events. Combined, these patterns can indicate milder forms of sleep-disordered breathing, possible presence of loop-gain and diminished arousal threshold, as well as more severe cases of sleep apnea.
Selecting Patients for Oral Appliance
Oral appliances are typically recommended for:
- Patients with mild to moderate OSA
- Patients who do not tolerate CPAP
- Patients who request treatment of primary snoring (without obstructive sleep apnea)14

Obstructive sleep apnea pathogenesis is multifactorial (i.e., patients have OSA for different reasons). Several nonanatomic factors including inadequate upper-airway muscle function, a large ventilatory response to a respiratory disturbance (high loop gain), and low arousal threshold can occur in conjunction with compromised pharyngeal anatomy. A 2016 study by Edwards, et al found that some of these factors may impact the success of oral appliance therapy. Specifically, responders to therapy had a lower loop gain and less collapsible airway under passive conditions.15 Also, patients with a low arousal threshold (i.e., those who wake more easily in response to ventilatory instability) tend to respond poorly to CPAP therapy.
The predictive success of oral appliance therapy depends on more factors than the number of desaturations per hour. Some oximetry reporting tools have looked at waveform patterns to indicate likelihood of low arousal threshold and high loop-gain, which may impact the patients’ likelihood of responding well to CPAP and oral appliance therapy.
OSA with Patients with severe ventilatory instability or high loop gain may experience less success with oral appliance therapy.16 Sleep, increased time delay, and increased tendency for the system to over respond (“underdamping”) are all known to promote an unstable breathing pattern though an increased systems response; “loop gain”.17 The increased time delay results in profound desaturations followed by late arousal and recovery in a recurrent pattern of ventilatory instability. In the example seen in Figure 3, characteristics of OSA with Severe Ventilatory Instability often include a clinically significant RDI, moderate to high Cycling Time, and high Cycling Severity.18 Conversely, patients with milder loop gain may respond well to oral appliance therapy as a first approach to treatment.
In figure 4, characteristics of OSA with Hyper-Arousal often include a clinically significant RDI, moderate to high Cycling Time, and low Cycling Severity. As is shown in the figure to the left, the patient experiences an arousal due to minimal upper airway obstruction, takes a deep “Startle breath” (ventilation overshoot), which is followed by a compensatory drop in ventilation & airway tone (ventilation undershoot), resulting in another brief obstruction, causing arousal, perpetuating the cycle. Patients experiencing this type of hyper arousal associated with milder desaturations may have poor response to CPAP therapy and therefore, may achieve better adherence with oral appliance if CPAP fails.12
Once patients have been identified as potentially having sleep related breathing disorders, most insurance companies require diagnosis by a home sleep test or in lab sleep study. The dentist may wish to share the findings of oximetry testing with a sleep specialist to work with the patient to find the most suitable path for treatment. The American Academy of Sleep Medicine recommends oral appliances be used with patients with mild to moderate sleep related breathing disorders, especially those intolerant of PAP, as well as for use with primary snoring.14
Conclusion
Overall, any health screener is used to indicate the next step – which ranges from no treatment for those with no risk to the next test for people at high risk of having the disease being looked for. Choosing the correct pulse oximeter can better identify patients with sleep related breathing disorders. By correctly identifying these patients, the proper sleep therapies and treatment can be offered. High resolution pulse oximetry using technological advancements shows better detection in identifying these patients than using subjective screening alone.
Read Dr. Ronald Prehn’s article that discusses the benefits of physicians prescribing overnight pulse oximetry testing to pre-screen for OSA here.
References
- Frost and Sullivan, “Hidden Health Crisis Costing America Billions,” American Academy of Sleep Medicine, Mountain View, CA, 1996.
- T. U. P. S. T. Force, “Screening for Obstructive Sleep Apnea in Adults,” JAMA, vol. 317, no. 4, pp. 407-414, 2017.
- L. M. A. P. M. R.Pateld, “The effectiveness of an obstructive sleep apnea screening and treatment program in patients with type 2 diabetes,” Diabetes Research and Clinical Practice, vol. 134, pp. 145-152, 2017.
- S. Mallampati, S. Gatt, L. Gugino, S. Desai, B. Waraksa, D. Freiberger and P. Liu, “A clinical sign to predict difficult tracheal intubation: a prospective study,” Canadian Anaesthetists’ Society Journal, vol. 32, no. 4, pp. 429-434, 1985.
- C. Hukins, “Mallampati Class Is Not Useful in the Clinical Assessment of Sleep Clinic Patients,” Journal of Clinical Sleep Medicine, vol. 6, no. 6, pp. 545-549, 2010.
- John Hopkins Medicine, “Pulse Oximetry,” https://www.hopkinsmedicine.org/healthlibrary/test_procedures/pulmonary/pulse_oximetry_92,p07754, 2019.
- R. T. L. R. M. G. S. L. A. D. L. D. F. K. L. E. K. Arthur Dawson, “Type III home sleep testing versus pulse oximetry: is the respiratory disturbance index better than the oxygen desaturation index to predict the apnoea-hypopnoea index measured during laboratory polysomnography?,” BMJ Open, pp. 5:e007956. doi: 10.1136/bmjopen-2015-007956, 2015.
- W. T. W. F. A. M. R. B. E. H. W. W. a. J. R. J. Vazquez, “Automated analysis of digital oximetry in the diagnosis of obstructive sleep apnoea,” Thorax, vol. 55, no. 4, pp. 302-307, 2000.
- B. S. S. E. T. P. W. B. N. Bohning, “Comparability of pulse oximeters used in sleep,” Physical Measurement, vol. 31, pp. 875-888, 2010.
- M. K.-R. A. I. R. W. B. T. B. J. Troy J. Cross, “The Impact of Averaging Window Length on the “Desaturation” Indexes Obtained Via Overnight Pulse Oximetry at High Altitude, Sleep,” Sleep, vol. 38, no. 8, p. 1331–1334, 1 August 2015.
- “Comparability of pulse oximeters used in sleep medicine for the screening of OSA,” Physiological Measurement, vol. 31, no. 7, pp. 875-888, 2010.
- L.-A. T. M. T. S. P. L. P. M. Mohamed El Shayeb MD MSc, “Diagnostic accuracy of level 3 portable sleep tests versuslevel 1 polysomnography for sleep-disordered breathing:a systematic review and metanalysis,” CMAJ, vol. 186, no. 1, pp. E25-E51, 2004.
- Patient Safety, “Patient Safety,” 2018. [Online]. Available: www.patientsafetyinc.com. [Accessed 19 January 2019].
- P. a. P. o. S. M. (. Edition, Principles and Practice of Sleep medicine, 5th ed., W.B. Saunders, 2011, pp. 1206-1218.
- M. M. Kannan Ramar, D. Leslie C. Dort, D. Sheri G. Katz, M. Christopher J. Lettieri and M. Christopher G. Harrod, “Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015,” Journal of Clinical Sleep Medicine, vol. 15, no. 1, 2015.
- C. S. C. J. E. D. Osman AM, “Obstructive sleep apnea: current perspectives,” Nature and Science of Sleep, vol. 2018, no. 10, pp. 21-34, 2018.
- C. A. S. L. S. A. S. S. A. J. R. L. O. D. P. W. G. S. H. A. W. Bradley A. Edwards, “Upper-Airway Collapsibility and Loop Gain Predict the Response to Oral Appliance Therapy in Patients with Obstructive Sleep Apnea,” Am J Respir Crit Care Med, vol. 194, no. 11, pp. 1413-1422, 2016.
- M. Y. D. T. Kimgman Strohl, “Loope Gain and Sleep related breathing disorders,” Current Respiratory Medicine Reviews, 2007.
- D. Lawrence Lynn, “Occult Arousal Failure,” in Ohio Sleep Doctors, Columbus, 2012.
- Q. S. Aurora RN, “Quality measure for screening for adult obstructive sleep apnea by primary care physicians.,” J Clin Sleep Med, vol. 12, no. 8, pp. 1185-1187, 2016.
- F. B. Y. M. P. L. M. S. A. C. P. Frances Chung, “STOP Questionnaire,” Anesthesiology, vol. 108, pp. 812-21, 2008.
 Craig Pickerill is the CEO of Patient Safety, Inc. (
Craig Pickerill is the CEO of Patient Safety, Inc. (