CE Expiration Date: January 31, 2028
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 730
Educational Aims
Once the cranial nerves are memorized during anatomy instruction in professional school, day-to-day awareness tends to be limited to nocioception and dysfunction. What may be underappreciated is the role the trigeminal nerve plays in facial growth and development and ongoing function. This self-instructional course for dentists reveals how nasal breathing, sleep-disordered breathing, and functional anomalies are all tied to the fifth cranial nerve, and how comprehensive head-and-neck medicine cannot be practiced without a thorough understanding of its contribution.
Expected Outcomes
Dental Sleep Practice subscribers can answer the CE questions online to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
- Cite several ways proper growth and development is tied to the functions of the trigeminal nerve.
- Appreciate the bidirectional influence of the trigeminal and nasal breathing.
- Consider how diagnosis, evaluation, treatment, and follow-up are intimately involved with the anatomy and function of the fifth cranial nerve.
Drs. Karen Parker Davidson and Donald R. Moeller delve into the functions for the trigeminal nerve and its importance to the processes that influence overall health, sleep quality, and breathing efficiency.

by Karen Parker Davidson, DHA, MSA, MEd, MSN, APRN, and Donald R. Moeller, DDS, MA, MD, Lieutenant Colonel US Army (retired)
Introduction
The trigeminal nerve, the largest and most complex of the cranial nerves, is often seen as the sensory powerhouse of the face. Its vast reach into the oral, nasal, and craniofacial structures makes it central to many physiological processes, from chewing and sensation to breathing and facial growth. Yet, its influence extends beyond simple sensory functions. In the context of facial growth and nasal breathing, the trigeminal nerve plays a crucial role in shaping development and function in ways that affect not only the structure of the face but also overall health, sleep quality, and breathing efficiency.1
This article delves into how the trigeminal nerve contributes to facial growth and development, its impact on nasal breathing, and the implications for dental sleep medicine. By understanding this vital nerve’s role, dental and medical professionals can better address disorders linked to nasal obstruction, sleep-disordered breathing, and developmental anomalies.
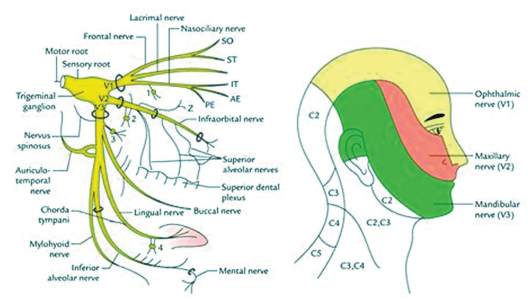
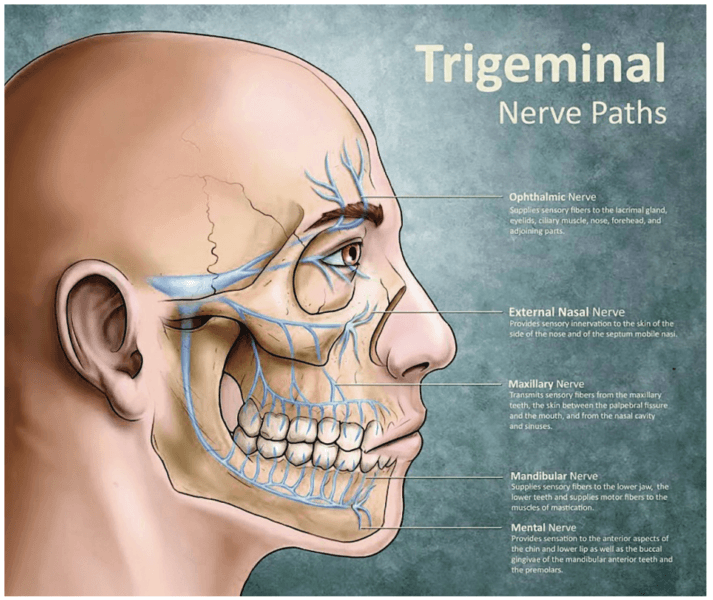
Anatomy of the Trigeminal Nerve
The trigeminal nerve (cranial nerve V) is the largest and most intricate of the cranial nerves, serving essential sensory and motor roles in the face, jaws, and associated structures. It branches into three main divisions: the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves. Each division is responsible for innervating specific regions of the face. The ophthalmic division (V1) provides sensory input to the forehead, scalp, upper eyelid, and parts of the nose. The maxillary division (V2) carries sensory signals from the midface, including the cheeks, upper lip, upper teeth, and nasal cavity, while the mandibular division (V3) has both sensory and motor functions, innervating the lower lip, jaw, and teeth, and controlling the muscles involved in mastication (chewing).1
The trigeminal nerve’s sensory functions are processed in its nuclei, which are located in the brainstem. These nuclei can be divided into three parts: the mesencephalic nucleus, chief sensory nucleus, and spinal trigeminal nucleus.2 The mesencephalic nucleus, located in the midbrain, is primarily responsible for proprioception, which is the body’s ability to sense the position of the jaw and muscles during activities like chewing.3 The bite force and pressure is detected in the afferent neural feedback loop from the V3 to the V2, also known as the V2-V3 Bio Feedback Loop, that impacts nasal function discussed later in the article. The chief sensory nucleus, found in the pons, processes sensations such as fine touch and pressure from the face. The spinal trigeminal nucleus, which extends from the pons into the upper spinal cord, processes sensations related to pain and temperature.
The motor functions of the trigeminal nerve stem from its motor nucleus, which is also located in the pons. This motor component controls the muscles of mastication, including the masseter, temporalis, and pterygoid muscles, facilitating essential functions like chewing and biting. In addition, the mandibular branch (V3) supplies motor fibers to other small muscles, such as the tensor tympani, involved in sound dampening, and the tensor veli palatini, which opens the auditory tube during swallowing.
Beyond simple sensory and motor functions, the trigeminal nerve is involved in reflexes that help protect the face and maintain facial integrity. The jaw jerk reflex is a monosynaptic reflex that tests the integrity of the trigeminal nerve, where a tap on the chin causes the jaw to jerk upward. The corneal reflex involves both the trigeminal and facial nerves; when the cornea is stimulated (sensed by V1), the facial nerve triggers a blink response to protect the eye. Similarly, the trigeminal nerve is crucial for the sneeze reflex, where irritation of the nasal mucosa (innervated by V2) leads to a coordinated response involving multiple nerves, causing a sneeze to expel irritants.
The trigeminal nerve interacts with many other cranial and peripheral nerves, forming complex networks that regulate sensory and motor functions in the face, neck, and oral cavity. It works in close association with the facial nerve (cranial nerve VII) in protective reflexes like blinking. It also coordinates with the glossopharyngeal (cranial nerve IX) and vagus nerves (cranial nerve X) in reflexes related to swallowing and the gag reflex, all which I call the hitchhikers of the trigeminal nerve. These interactions are essential for maintaining both voluntary and involuntary facial movements, and play a role in breathing and sleep patterns. In essence, the vagus nerve is not stimulated, but feeding off of neural pathway of the trigeminal nerve in the nasobronchial reflexes.3 Breathing exercises are an example; the sympathetic charge in the nasal mucosa is withdrawn allowing the parasympathetic nervous system to become dominant and initiate a vagus response.
In addition to these reflexes, the trigeminal nerve is part of both ascending and descending neural pathways.4 Sensory information collected by the trigeminal nerve is sent through these pathways to the thalamus and the primary sensory cortex, allowing the brain to process sensations such as pain, temperature, and touch. Motor signals originating in the brain are sent down to the trigeminal nerve’s motor nucleus, enabling voluntary movements like chewing and jaw opening.
Understanding the intricate anatomy and physiology of the trigeminal nerve is clinically significant. Trigeminal neuralgia, for example, is a condition characterized by intense facial pain due to dysfunction of the trigeminal nerve, often triggered by simple sensory stimuli. Similarly, the nerve’s involvement in temporomandibular joint (TMJ) disorders shows how dysfunction in the mandibular division can contribute to jaw misalignment and pain. Additionally, sleep-disordered breathing conditions, such as obstructive sleep apnea, may be exacerbated by trigeminal nerve dysfunction, particularly if nasal airflow is compromised.5
Given these vast sensory and motor responsibilities, the trigeminal nerve is vital for integrating sensory feedback with motor control, allowing for critical functions like chewing, speaking, and breathing to operate harmoniously. But beyond these immediate functions, the trigeminal nerve is intimately connected to the processes of growth, development, and airway management.
The Trigeminal Nerve and Facial Growth
Facial growth is a complex interplay of genetic programming, environmental influences, and functional forces. One of the most significant drivers of facial development is the functional stimulus provided by the muscles and bones of the face. The trigeminal nerve plays a crucial role in this process through both its sensory and motor functions.6
Mastication and Skeletal Development
The mandibular branch of the trigeminal nerve innervates the muscles responsible for chewing (mastication), including the masseter, temporalis, and pterygoid muscles. The forces generated during mastication create mechanical stresses on the bones of the face, especially the maxilla, mandible, and zygomatic bones.7 These stresses stimulate bone growth and remodeling through a process known as mechanotransduction, in which physical forces are translated into cellular responses that drive bone formation and adaptation. New studies found the trigeminal nerve and the cerebellum stabilize the jaw while running, walking, and jogging, since the muscles change in each activity, meaning the head and neck position is naturally monitored.
Proper chewing in childhood and adolescence is essential for the healthy development of the jaws and facial structure.8 A diet that requires vigorous chewing (such as fibrous, unprocessed foods) stimulates muscle and bone development, while a soft diet can lead to underdeveloped jaws, malocclusion, and even airway constriction.9 Since the trigeminal nerve controls the muscles of mastication, it is a key player in this developmental process.
Sensory Feedback and Bone Remodeling
The sensory branches of the trigeminal nerve, particularly the maxillary and mandibular branches, provide feedback from the teeth, gums, and surrounding tissues.10 This sensory feedback is essential for coordinating the growth and adaptation of the craniofacial skeleton. Sensory nerve fibers interact with bone cells (osteocytes) and signaling pathways that regulate bone remodeling, ensuring that the bones of the face grow in harmony with functional demands.11
In addition, sensory inputs from the teeth and temporomandibular joint (TMJ) influence the growth of the mandible and maxilla. Orthodontic and dentofacial orthopedic treatments often rely on manipulating these forces to guide facial growth, and understanding the trigeminal nerve’s role can improve the precision and efficacy of such interventions that affect patients who make up the 60% of the population with high nasal resistance and TMJ issues. As stated in the past regrading an increased pressure within the sinus cavities, it is not the heightened pressure disrupting the balance of forces in and around the jaw joint, potentially leading to TMJ symptoms, but the V2-V3 biofeedback loop.
The Trigeminal Nerve and Nasal Function
Nasal function plays a vital role in overall health, influencing everything from oxygenation and cardiovascular function to sleep quality and cognitive performance. The trigeminal nerve is deeply involved in regulating nasal airflow and ensuring proper nasal function in the specialty of Functional Rhinology.12,13
Nasal Sensory Innervation
The ophthalmic (V1) and maxillary (V2) branches of the trigeminal nerve provide sensory innervation to the nasal cavity. This sensory input allows the body to detect changes in airflow, temperature, and humidity, which helps regulate breathing patterns. For example, when cold air enters the nasal passages, the trigeminal nerve senses the temperature change and signals the body to warm and humidify the air before it reaches the lungs. This process is essential for maintaining optimal respiratory function.
Moreover, the trigeminal nerve’s sensory feedback helps protect the nasal passages from harmful irritants. When the nerve detects irritants like dust or allergens, it triggers reflex actions such as sneezing or nasal congestion to prevent these particles from entering the lungs. This protective mechanism is crucial for maintaining airway health and function.
Regulation of Nasal Airflow
The trigeminal nerve also plays a role in regulating the tone of the nasal mucosa and blood vessels. Through autonomic reflex pathways, the trigeminal nerve influences vasoconstriction and vasodilation in the nasal passages, helping to control the resistance of the nasal airway. This regulation is particularly important during sleep, when nasal congestion can exacerbate conditions such as obstructive sleep apnea (OSA) in the prone and supine positions, especially in REM sleep where nasal resistance is at its highest point.
Sleep-disordered breathing, especially in children, can have long-term effects on facial growth and development. Chronic mouth breathing, often caused by nasal obstruction, alters the normal growth patterns of the face and jaws, leading to a long, narrow face, an underdeveloped maxilla, and a retrusive mandible. These structural changes can further impair breathing, creating a vicious cycle. The trigeminal nerve’s role in maintaining nasal patency is therefore crucial for preventing these developmental issues.
Nasal Function and Its Importance
Proper nasal breathing is essential for overall health. The nose filters, warms, and humidifies the air before it reaches the lungs. Any disruption in nasal function can lead to breathing difficulties and associated health issues. The trigeminal nerve’s role in maintaining nasal sensation is thus vital for ensuring effective nasal breathing. The trigeminal nerve’s sensory input plays a crucial role in regulating breathing. Mechanoreceptors and chemoreceptors in the nasal cavity and sinuses, innervated by the maxillary branch (V2), detect changes in airflow, pressure, and the presence of irritants. This sensory information is essential for maintaining effective nasal breathing and triggering reflexes that protect the respiratory system. Malocclusions and other orthodontic issues can impact nasal breathing. For example, a high-arched palate can reduce the nasal airway space, leading to breathing difficulties however, volume, or a bigger nose does not correlate to better nasal function. Orthodontic interventions can help expand the palate, thereby improving nasal airflow. Understanding the interplay between dental structures and nasal function, mediated by the trigeminal nerve, is crucial for comprehensive orthodontic care.
Clinical Implications for Dental Sleep Medicine
Understanding the role of the trigeminal nerve in facial growth and nasal breathing has significant implications for dental sleep medicine. Here are several key takeaways:
Airway Development and Breathing Disorders During Sleep
Children with nasal obstruction or chronic mouth breathing are at risk for developing malocclusions, skeletal disharmony, and sleep-disordered breathing conditions such as OSA. Early intervention aimed at restoring nasal breathing and encouraging proper jaw growth is essential. Dental appliances, myofunctional therapy, and orthodontic treatments can guide facial growth and support proper airway development. These interventions often rely on stimulating the muscles and bones innervated by the trigeminal nerve to promote healthy development.
Trigeminal Neuralgia and Sleep Disturbances
Disorders of the trigeminal nerve, such as trigeminal neuralgia, can cause chronic facial pain and disrupt sleep. While trigeminal neuralgia is primarily characterized by episodes of intense facial pain, the associated discomfort and stress can interfere with sleep quality. Addressing these issues through medical or surgical interventions can significantly improve patients’ sleep and overall well-being.
4-phase Rhinomanometry and Trigeminal Function
A biofeedback loop in the context of breathing involves continuous monitoring and regulation of respiratory parameters and nasal function to maintain homeostasis. The trigeminal nerve’s sensory input is a critical component of this loop, providing real-time feedback to the brain about the state of the nasal passages and airflow. When sensory receptors detect a change, such as an obstruction or irritant in the nasal cavity or changes in bite force and pressure, signals are sent via the trigeminal afferent neural pathway to the brainstem. This is more noticeable when using a specialized oral neuromodulating device. The brainstem integrates this information and initiates appropriate responses, such as adjusting the rate and depth of breathing. Increasing nasal resistance, or triggering a sneeze to expel the irritant. Observation and first identified during my time in Dr. Moeller’s clinic, the V2-V3 afferent biofeedback loop in rhinomanometry tracings during active breathing further emphasizes the role of CN5 and vertical height; this novel discovery showed it wasn’t the volume changes and titration that improved the airway in a veteran with PTSD, but the quantifiable variations in transnasal pressure change as a biomarker.
Rhinomanometry, a diagnostic tool that measures nasal airflow and resistance, can provide valuable insights into the function of the nasal passages and the role of the trigeminal nerve in regulating airflow, especially with the involvement of the oral cavity. In cases where nasal obstruction is suspected, rhinomanometry can help identify whether the obstruction is due to structural issues, inflammation, or autonomic dysfunction influenced by the trigeminal nerve.
Orthodontics and Facial Growth and Neural Modulation
In orthodontics, treatments such as rapid maxillary expansion (RME) are designed to stimulate the maxilla’s growth and improve nasal airflow. These treatments may also influence the trigeminal nerve’s sensory feedback mechanisms, helping guide bone remodeling and improve facial symmetry, as well as nasal function as a response to treatment to avoid overexpansion and alterations in the pneumatization of the maxillary sinuses. As understanding of the trigeminal nerve’s role in growth and function expands, orthodontic and orthopedic approaches may become more refined, offering targeted interventions for facial growth and airway management.
Conclusion
The trigeminal nerve’s role in facial growth and nasal breathing is both profound and multifaceted. From guiding the development of the craniofacial skeleton to regulating nasal airflow and reflexes, this nerve is essential to many processes that influence overall health, sleep quality, and breathing efficiency. For dental sleep medicine professionals, a deep understanding of trigeminal nerve function offers new avenues for diagnosis, treatment, and intervention in cases of sleep-disordered breathing, malocclusion, and developmental anomalies. By addressing the root causes of these issues, clinicians can help patients achieve better health outcomes, both in their facial structure and their breathing function. The trigeminal nerve is integral not only in sensory and motor functions but also in regulating various physiological processes, including breathing. This paper extends the exploration of the trigeminal nerve’s role by delving into the afferent neural pathway and the biofeedback loop involved in active breathing. Understanding how these processes are measured is crucial for developing advanced diagnostic and therapeutic strategies in fields such as dentistry, orthodontics, and respiratory medicine..
Future Directions
Future research should focus on further elucidating the intricate connections between the trigeminal nerve and various dental and orthodontic conditions. Advances in imaging techniques and neurophysiological studies will enhance our understanding of these relationships, leading to improved diagnostic and therapeutic strategies. Additionally, interdisciplinary approaches combining dentistry, orthodontics, and otolaryngology will foster a more comprehensive understanding of the trigeminal nerve’s role in craniofacial health. This should also focus on incorporating 4-phase rhinomanometry to further elucidate the role of the trigeminal nerve in the dental practice. Interdisciplinary collaboration between neuroscientists, otolaryngologists, and respiratory specialists will be essential in advancing our understanding of these complex neural mechanisms and improving patient care.
The trigeminal nerve can be a culprit for craniofacial pain. Find out how the head, neck, and trigeminal nerve can be involved in craniofacial pain and how building partnerships with physicians can help you to provide the best care for your patients in this article by Dr. Mayoor Patel. https://dentalsleeppractice.com/building-partnerships-with-physicians-when-treating-craniofacial-pain/
References
- Huff T, Weisbrod LJ, Daly DT. Neuroanatomy, Cranial Nerve 5 (Trigeminal). In: StatPearls. Treasure Island (FL): StatPearls Publishing; April 20, 2024.
- Price S, Daly DT. Neuroanatomy, Trigeminal Nucleus. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539823/
- Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurements: a literature review. Eur J Dent. 2010;4(2):223-232.
- Baraniuk JN, Merck SJ. Nasal reflexes: implications for exercise, breathing, and sex. Curr Allergy Asthma Rep. 2008;8(2):147-153. doi:10.1007/s11882-008-0025-7
- Bindu B, Singh GP, Chowdhury T, Schaller B. Rhinitis and sleep disorders: The trigeminocardiac reflex link?. Med Hypotheses. 2017;103:96-99. doi:10.1016/j.mehy.2017.04.019
- Cobo, J.L. et al. Connections between the facial and trigeminal nerves: Anatomical basis for facial muscle proprioception JPRAS Open. 2017;12: 9 – 18.
- Moss ML, Salentijn L. The primary role of functional matrices in facial growth. Am J Orthod. 1969;55(6):566-577. doi:10.1016/0002-9416(69)90034-7
- Oral Health in America: Advances and Challenges [Internet]. Bethesda (MD): National Institute of Dental and Craniofacial Research(US); 2021 Dec. Section 2A, Oral Health Across the Lifespan: Children. Available from: https://www.ncbi.nlm.nih.gov/books/NBK578299/
- Ramirez-Yañez, G.O. (2019). Craniofacial Growth and Development. In: Liem, E. (eds) Sleep Disorders in Pediatric Dentistry . Springer, Cham. https://doi.org/10.1007/978-3-030-13269-9_3
- Carlson, D. S. (2005). Growth and Development of the Jaws: Influence of Muscle Function. American Journal of Orthodontics and Dentofacial Orthopedics, 128(5), 533-540.
- Wu Y, Lan Y, Mao J, Shen J, Kang T, Xie Z. The interaction between the nervous system and the stomatognathic system: from development to diseases [published correction appears in Int J Oral Sci. 2023 Sep 11;15(1):39. doi: 10.1038/s41368-023-00250-3]. Int J Oral Sci. 2023;15(1):34. Published 2023 Aug 15. doi:10.1038/s41368-023-00241-4
- Vogt K, Parker-Davidson K. Measurement of Nasal Obstruction: Rhinomanometry as basic method in functional rhinology. Facial Plast Surg. 2024;40(3):314-322. doi:10.1055/a-2218-5883
- Parker Davidson, K. Breathe Through Your Nose, Don’t Pay Through It: The Impact the Healthcare Industry Has on Nasal Function and How We Breathe. PeeDee Publishing; 2022.
 Dr. Karen Parker Davidson is a graduate of the University of North Carolina at Chapel Hill School of Nursing, attended the University of North Dakota College of Nursing Family Nurse Practitioner program, completed three master’s degree programs at Central Michigan University and University of Phoenix, earned her doctorate in Health Administration with a focus in Health Policy, also from Central Michigan University, and is currently pursuing a PhD in Business Administration with a focus on International Business. With more than three decades of clinical and medical device industry experience in various roles, she also served as a Flight Nurse and Critical Care Nurse in the United States Air Force Reserves with the 315th and 459th Air Wings. She is an adjunct professor, dissertation chair, and health policy SME at Liberty University’s Division of Public & Community Health, School of Health Sciences, and School of Business, and is adjunct faculty at Central Michigan University, School of Health Professions. She is a member of the American College of Healthcare Executives and the National Association of Clinical Nurse Specialists.
Dr. Karen Parker Davidson is a graduate of the University of North Carolina at Chapel Hill School of Nursing, attended the University of North Dakota College of Nursing Family Nurse Practitioner program, completed three master’s degree programs at Central Michigan University and University of Phoenix, earned her doctorate in Health Administration with a focus in Health Policy, also from Central Michigan University, and is currently pursuing a PhD in Business Administration with a focus on International Business. With more than three decades of clinical and medical device industry experience in various roles, she also served as a Flight Nurse and Critical Care Nurse in the United States Air Force Reserves with the 315th and 459th Air Wings. She is an adjunct professor, dissertation chair, and health policy SME at Liberty University’s Division of Public & Community Health, School of Health Sciences, and School of Business, and is adjunct faculty at Central Michigan University, School of Health Professions. She is a member of the American College of Healthcare Executives and the National Association of Clinical Nurse Specialists. Dr. Donald R. Moeller graduated from San Jose State University with a bachelor’s degree in Biological Science, entered dental school at the University of California San Francisco, and graduated with a Doctor of Dental Surgery degree and then joined the US Army Dental Corps. He completed his Residency in Oral and Maxillofacial Surgery (OMS) at the Walter Reed Army Medical Center during which time he was also involved in PhD Mentored Research at the Walter Reed Army Institute of Dental Research. This early experience in Surgical Trauma Research motivated him to obtain a graduate degree in Biological Sciences with a Cellular Biology emphasis. After retiring as Chief of Oral and Maxillofacial Surgery at Martin Army Hospital Fort Moore Georgia, Dr. Moeller entered the University of Alabama Medical School at Birmingham where he received a Doctor of Medicine degree. Dr. Moeller completed his Transitional Medical Residency at the Columbus Medical Center and then briefly served as an Assistant Professor of OMS at Augusta University.
Dr. Donald R. Moeller graduated from San Jose State University with a bachelor’s degree in Biological Science, entered dental school at the University of California San Francisco, and graduated with a Doctor of Dental Surgery degree and then joined the US Army Dental Corps. He completed his Residency in Oral and Maxillofacial Surgery (OMS) at the Walter Reed Army Medical Center during which time he was also involved in PhD Mentored Research at the Walter Reed Army Institute of Dental Research. This early experience in Surgical Trauma Research motivated him to obtain a graduate degree in Biological Sciences with a Cellular Biology emphasis. After retiring as Chief of Oral and Maxillofacial Surgery at Martin Army Hospital Fort Moore Georgia, Dr. Moeller entered the University of Alabama Medical School at Birmingham where he received a Doctor of Medicine degree. Dr. Moeller completed his Transitional Medical Residency at the Columbus Medical Center and then briefly served as an Assistant Professor of OMS at Augusta University.