CE Expiration Date: November 26, 2021
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 010
Educational aims
The physiology of respiration has a direct effect on every body system. The airway therapy provided by dentists enables respiration to return to homeostasis, so the providing dentists must be aware of how that system works in the body. The importance of nasal breathing goes far beyond the need to avoid dry mouth.
Expected outcomes
Dental Sleep Practice subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article.
Before taking the quiz, read part 1 of this series here.
Correctly answering the questions will allow the reader to:
- Be able to discuss the balance between O2 and CO2 in respiration and how it is affected by breathing changes
- Know about how to affect hypocapnia in a positive way
- Appreciate that OSA is only part of a group of SRBD that must be accounted for by the provider group for each patient
Editor’s Intro: Obstructive sleep apnea (OSA): Dentists play a pivotal role in successful treatment.
by Allen J. Moses, DDS; Elizabeth T. Kalliath, DMD; and Gloria Pacini, RDH
Introduction
OSA is a breathing disorder. Breathing is essential to support life. Air must get to and from the lungs for oxygenation and physiological exchange and conditioning of gases. Noses and lungs have a very rich blood supply consisting of venules, arterioles and capillaries. Each one of these is a smooth muscle-controlled group regulated by CO2 levels.
The Physiological Consequences of Mouth Breathing
Breathing supplies oxygen to all 300 trillion body cells, removes excess CO2 and certain waste materials. Earth’s atmosphere contains approximately 21% oxygen. Human bodies require 6.0-6.5% O2. There is more O2 in the atmosphere than the human body requires. Storing O2 in the body is not necessary. Earth’s atmosphere normally contains .03% CO2. 100% saturation of human blood for CO 2 is 6.0 – 6.5%. Therefore, more CO2 is required in the body than is present in the normal atmosphere. The body needs to obtain CO2 to sustain life. The body acquires CO2 by breathing. CO2 is stored in the blood and lungs.1
2 is 6.0 – 6.5%. Therefore, more CO2 is required in the body than is present in the normal atmosphere. The body needs to obtain CO2 to sustain life. The body acquires CO2 by breathing. CO2 is stored in the blood and lungs.1
The optimum operating range for human body is between ph 7.35 – 7.45. At pH <6.8 or pH >7.8, cells die. The acid-base balance is regulated by breathing and conversion of CO2 into bicarbonate (HCO3) or carbonic acid (H2CO3). The lungs excrete over 10,000 mEq of carbonic acid per day. The kidneys excrete less than 100 mEq per day. Therefore, by altering alveolar ventilation and eliminating CO2, great control over the acid-base balance can be exercised via mouth breathing. A low level of CO2 results in alkalosis. Mouth breathing accelerates the breathing rate. Hyperventilation results in respiratory alkalosis.
 The blood becomes alkaline when the pH is elevated above 7.45. The O2 becomes bound to hemoglobin (Hg) and is not released to cells. This is called the Bohr Effect. As CO2 levels in arterial blood drop, the strength of the bond between O2 and Hg increases, reducing the amount of O2 available to cells. Patients can have a normal blood oxygen level but if the CO2 level is too low, the oxygen is not released to the body’s cells.
The blood becomes alkaline when the pH is elevated above 7.45. The O2 becomes bound to hemoglobin (Hg) and is not released to cells. This is called the Bohr Effect. As CO2 levels in arterial blood drop, the strength of the bond between O2 and Hg increases, reducing the amount of O2 available to cells. Patients can have a normal blood oxygen level but if the CO2 level is too low, the oxygen is not released to the body’s cells.
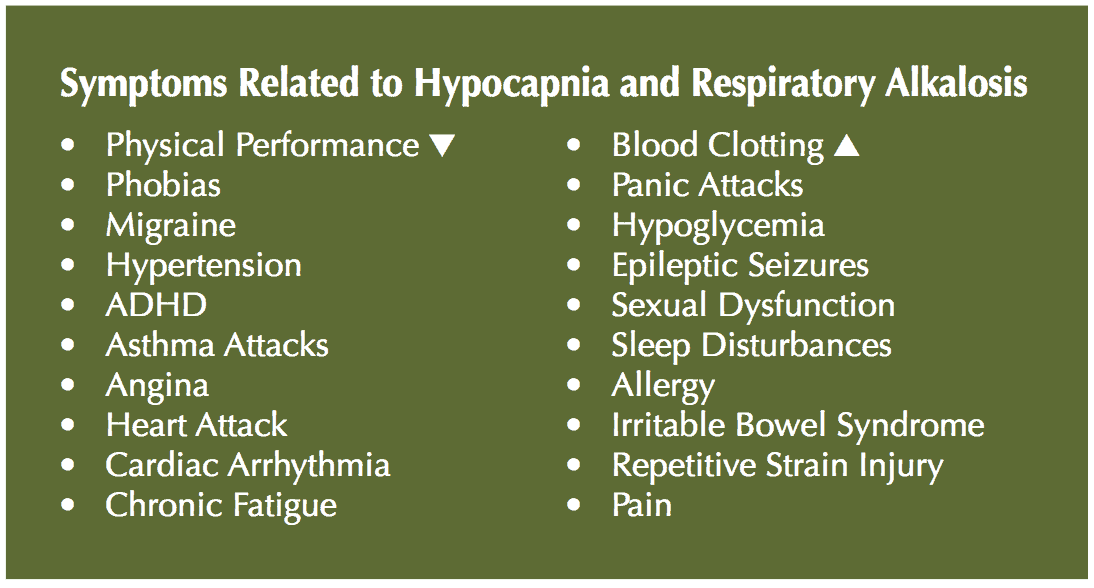
It is important to monitor the breathing rate. At 40 mg of mercury pressure (Hg), the diaphragm moves. This occurs at 6.5% CO2 in lungs. Humans are triggered from birth at 40 mg. Below 35 mg Hg pressure is considered hypocapnia. Ideal breath rate is 6 – 10 breaths/minute. Rapid breathing is 14 – 18 breaths/minute. Rapid breathing resulting from mouth breathing and depletes CO2. Hypocapnia, respiratory alkalosis, poor binding of O2, smooth muscle spasm, enuresis, HBP, snoring, hypoxia, reduced energy, and disturbed sleep can result from overbreathing.2
 Mouth breathing bypasses the filtration, warming and humidification system of the nose. The mouth can deliver 5 times as much air to the lungs but the air is unconditioned and dry. The bronchiolar reflex shrinks the airway passage to reduce quantity of irritating air. Breathing becomes rapid and shallow. Lung tissue produces mucus to protect itself. CO2 levels become lower (hypocapnia) and blood pH increases. Respiratory alkalosis ensues.
Mouth breathing bypasses the filtration, warming and humidification system of the nose. The mouth can deliver 5 times as much air to the lungs but the air is unconditioned and dry. The bronchiolar reflex shrinks the airway passage to reduce quantity of irritating air. Breathing becomes rapid and shallow. Lung tissue produces mucus to protect itself. CO2 levels become lower (hypocapnia) and blood pH increases. Respiratory alkalosis ensues.
Correct, diaphragmatic breathing behaviors can be taught.3 There are behavioral training methods and biofeedback methods. Results can be objectively measured by capnometry, measuring End Tidal CO2. Patients who have had surgery to treat obstructed nasal breathing often habitually mouth breathe afterward. They need to be retrained behaviorally to nasal breathe.
Dentists can treat hypocapnia related to overbreathing in several ways. Oral appliances can be used if their design is based on the premise that the more room they can create for the tongue to fit in the mouth, the less likely it is to collapse on the airway during sleep. Design of the oral appliance should enable the patient to comfortably keep the lips closed. Excellent oral appliances facilitate placement of the tongue as far forward as possible, even touching the lips. Excellent oral appliances allow placement of the tongue in the roof of the mouth with no interference from palatal acrylic.
There is good evidence that the myofunctional correction of breathing behaviors taught during the day persist at night. Behavioral retraining instruction on OSA patients given during the day for a thirty day period persisted at night when measured by PSG, according to studies by Puhan4 and Guimaraes.5 The success of this type of study will also be discussed in another paper in this series as substantiating OSA as a soft wired problem.
CPAP is interesting. It has the positive effect on hypocapnia of causing the CO2 level to rise because patients are forced to breathe against a positive pressure gradient and CPAP reduces the breath rate. CPAP can also have a negative effect when too much pressure from the nasal pillows causes the mouth to open. Too much pressure from a full face mask has been reported to cause central apneas and acidosis.

Conclusion
Diagnosis of OSA and treatment with CPAP and/or an oral sleep appliance may not put enough pieces of the puzzle in place to give the clinician a comprehensive picture of the patient’s health status. A diagnosis of OSA established solely by PSG, is a “rule-in” diagnosis with a narrow clinical focus. OSA is merely one of several sleep breathing disorders. As such, a diagnosis of OSA does not rule-out other possibilities such as chronic hyperventilation and its attendant co-morbidities such as respiratory alkalosis, hypocapnia, smooth muscle spasm, hypoglycemia, asthma attacks, ADHD, cardiac arrhythmias, chronic heart diseases and type 2 diabetes. It may appear that the patient is merely nonresponsive or noncompliant to sleep apnea treatment. Diagnosis of chronic hyperventilation/hypocapnia is easily accomplished by PSG, history, examination and a capnometer study. Dentists should have familiarity with these modalities to either use them as treatment methodologies or be knowledgeable enough to refer patients to trained health specialists.
Treatment of hypocapnia/respiratory alkalosis/chronic hyperventilation can often be non-invasive and largely utilize cognitive behavior therapy and psychological re-education. The results of successful treatment of chronic hyperventilation can be very gratifying. Treatment of sleep disordered breathing is dependent on clinicians having a broad education and training in basic sciences as well as OSA, to apply that education to clinical experience. Dentists can play a pivotal role in both treatment and/or referral.


Learn more about obstructive sleep apnea (OSA)!
References
- Guyton AC, Hall JE, “Textbook of medical physiology” Chemical Control of Respiration; WB Saunders 1996 ed 9 527-528
- Kamel KS, Halperin ML, “Fluid Electrolyte and Acid-Base Physiology: Problem Based Approach”; Elsevier, 5 ed, 2017
- Buteyko Breathing Method. Shut your mouth and change your life, McKeown P, TEDx Galway, http://www.youtube.com/watch?v=mBqGS-vELs0
- Puhan M, Suarez, A, et.al. Didgeridoo playing as alternative treatment for obstructive sleep apnoea syndrome: randomized controlled study. BMJ 2006;332 (7536)266-270
- Guimares KC, Drager LF, et.al. Effects of oropharyngeal exercises of patients with moderate obstructive sleep apnea syndrome. Am J Crit Care Med 2009 v179 962-966.

 Dr. Allen Moses has had a dental practice in Sears/ Willis Tower for over 25 years and was assistant professor at Rush University for 15 years in the department of sleep research and clinical practice. He is the inventor of The Moses® intraoral sleep appliance distributed worldwide by Modern Dental Lab, and the Express4Sleep™. He has four US patents and has written more than 30 articles on sleep dentistry, facial pain and temporomandibular disorders.
Dr. Allen Moses has had a dental practice in Sears/ Willis Tower for over 25 years and was assistant professor at Rush University for 15 years in the department of sleep research and clinical practice. He is the inventor of The Moses® intraoral sleep appliance distributed worldwide by Modern Dental Lab, and the Express4Sleep™. He has four US patents and has written more than 30 articles on sleep dentistry, facial pain and temporomandibular disorders.