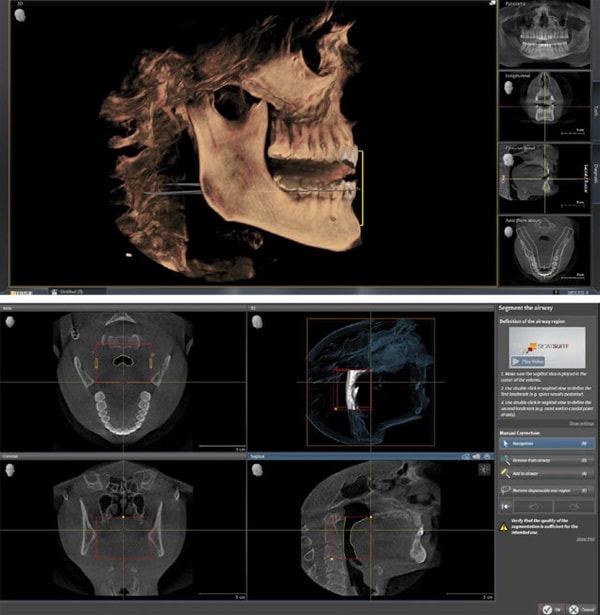
 A perfect, unobstructed, smooth-flowing, and properly functioning airway would be my wish for everyone. My second wish would be to treat the “root cause” of the compromised airflow, whether it be orthodontic expansion, surgically facilitated orthodontic treatment (SFOT), mandibular advancement surgery, rhinoplasty and sinus reconstruction, or maybe just eliminating allergens and learning to breathe through the nose again, or any combination thereof. But what about the patient for whom a mandibular advancement device is the appropriate treatment for better sleep and airway? (Figures 1-2) Whether temporary or long-term, there are patients who need an appliance to “help them get worse at the slowest possible rate,” as Bob Barkley so eloquently stated. The patient understands that they are compromised and could do more about their problem. Yet they don’t. But they might still need dentistry. Yet they are having their mandible pulled forward every night. And teeth might move. And skeletal structures might change. Why would we do more than “repair” them, addressing issues only as they arise? Why would we want to even discuss optimal treatment? Every patient is entitled to know what optimal is, the benefit, the likely consequences of suboptimal, and the compromises of anything less. The process for the dentist can still be systematic, interdisciplinary in nature, and somewhat predictable.
A perfect, unobstructed, smooth-flowing, and properly functioning airway would be my wish for everyone. My second wish would be to treat the “root cause” of the compromised airflow, whether it be orthodontic expansion, surgically facilitated orthodontic treatment (SFOT), mandibular advancement surgery, rhinoplasty and sinus reconstruction, or maybe just eliminating allergens and learning to breathe through the nose again, or any combination thereof. But what about the patient for whom a mandibular advancement device is the appropriate treatment for better sleep and airway? (Figures 1-2) Whether temporary or long-term, there are patients who need an appliance to “help them get worse at the slowest possible rate,” as Bob Barkley so eloquently stated. The patient understands that they are compromised and could do more about their problem. Yet they don’t. But they might still need dentistry. Yet they are having their mandible pulled forward every night. And teeth might move. And skeletal structures might change. Why would we do more than “repair” them, addressing issues only as they arise? Why would we want to even discuss optimal treatment? Every patient is entitled to know what optimal is, the benefit, the likely consequences of suboptimal, and the compromises of anything less. The process for the dentist can still be systematic, interdisciplinary in nature, and somewhat predictable.
The Dilemma
 Perfected occlusion, as Dawson describes it is “…simultaneous equal intensity contacts on all teeth when the condyle-disc assemblies are completely seated in their respective sockets,” and “the disclusion of all posterior teeth the moment the mandible moves from centric relation.”1 This sounds somewhat counterintuitive since pulling the mandible forward every night has long been known, and currently confirmed in the literature, to cause unpredictable changes, while opening the airway. (Figures 3-4) One 11-year study showed that, “clinically significant changes in occlusion were observed and were progressive in nature. Rather than reaching a discernible end-point, the dental side effects of MAS therapy continue with ongoing MAS use.”2 Maybe slightly less discouraging, yet an undeniable consequence that we have all seen to some extent, that is also in current literature, is that, “The use of MADs may lead to the development of TMD in a small number of patients. Nevertheless, these signs are most likely transient. Patients with pre-existing signs and symptoms of TMD do not experience significant exacerbation of those signs and symptoms with MAD use. Furthermore, these may actually decrease over time. POB (posterior open bite) was found to develop in 17.9 % of patients; however, only 28.6 % of these patients were aware of any bite changes.”3 So, how does one even begin to treatment plan possible treatment in such an unpredictable environment?
Perfected occlusion, as Dawson describes it is “…simultaneous equal intensity contacts on all teeth when the condyle-disc assemblies are completely seated in their respective sockets,” and “the disclusion of all posterior teeth the moment the mandible moves from centric relation.”1 This sounds somewhat counterintuitive since pulling the mandible forward every night has long been known, and currently confirmed in the literature, to cause unpredictable changes, while opening the airway. (Figures 3-4) One 11-year study showed that, “clinically significant changes in occlusion were observed and were progressive in nature. Rather than reaching a discernible end-point, the dental side effects of MAS therapy continue with ongoing MAS use.”2 Maybe slightly less discouraging, yet an undeniable consequence that we have all seen to some extent, that is also in current literature, is that, “The use of MADs may lead to the development of TMD in a small number of patients. Nevertheless, these signs are most likely transient. Patients with pre-existing signs and symptoms of TMD do not experience significant exacerbation of those signs and symptoms with MAD use. Furthermore, these may actually decrease over time. POB (posterior open bite) was found to develop in 17.9 % of patients; however, only 28.6 % of these patients were aware of any bite changes.”3 So, how does one even begin to treatment plan possible treatment in such an unpredictable environment?
Systematic Approach to Visualize Optimal Esthetics and Function
Understanding the current condition of the entire stomatognathic system and visualizing the ideal end result must always be a starting point. If we don’t begin with the optimal end in mind, how can we ever know what is possible and how any compromise might affect the otherwise optimal treatment? A systematic approach helps shed light beyond the confusing starting point. You might be refer to it as Global Diagnosis, Diagnostically Driven Treatment Planning, or Facially Generated Treatment Planning, to name a few. The name is less important than the process for treatment planning, ranging from simple to complex. When working from the face or from the outside in, “the outcome of the esthetic treatment plan will be enhanced without sacrificing the structural, functional and biological aspects of the patient’s dentition.”4 (Figure 5)
 A recent article describes a case study restoring a 29-year-old woman with a history of stomach-acid-related reflux and extensive loss of tooth structure, similar to what we see in many patients with airway or sleep issues. The author noted that the goal was to, “improve the prognosis in each of the four dental categories-periodontal, biomechanical, functional, and dentofacial, and that, “the treatment plan utilized a systematic approach to sequentially restore and protect the young woman’s dentition.”5 The verbiage is less important than the process. However, what might be more important when restoring a patient whose mandible is being held forward on a nightly basis is understanding and visualizing a stable physiologic position which will be challenged by the appliance.
A recent article describes a case study restoring a 29-year-old woman with a history of stomach-acid-related reflux and extensive loss of tooth structure, similar to what we see in many patients with airway or sleep issues. The author noted that the goal was to, “improve the prognosis in each of the four dental categories-periodontal, biomechanical, functional, and dentofacial, and that, “the treatment plan utilized a systematic approach to sequentially restore and protect the young woman’s dentition.”5 The verbiage is less important than the process. However, what might be more important when restoring a patient whose mandible is being held forward on a nightly basis is understanding and visualizing a stable physiologic position which will be challenged by the appliance.
 A fully-seated condylar position has been shown to be an optimal, albeit controversial in some circles, position at which to restore a patient when the joint space and disc are healthy. Several recent studies demonstrate that, “the condylar position is an important concern in maintaining or restoring temporomandibular harmony with the dentition and the position of the condyle in the glenoid fossa plays an important role in the stability of occlusion,”6 and that it, “contributes not only as a reference position to build optimal occlusion in artificial dentition, but is also related to sound periodontal health and stomatognathic function.”7 Visualizing the ideal function can be done using models to better understand the structure necessary to achieve the function and the likely compromises to suboptimal. (Figures 6-7) Once the ideal esthetics and function have been visualized, a key to restoring most patients, but especially patients wearing a MAD, is to involve the interdisciplinary team when discussing the ideal structure and supporting biology, to better understand the possible shortcomings due to the compromise of wearing the appliance, and maybe more important, options for carefully and predictably phasing the treatment. (Figure 8)
A fully-seated condylar position has been shown to be an optimal, albeit controversial in some circles, position at which to restore a patient when the joint space and disc are healthy. Several recent studies demonstrate that, “the condylar position is an important concern in maintaining or restoring temporomandibular harmony with the dentition and the position of the condyle in the glenoid fossa plays an important role in the stability of occlusion,”6 and that it, “contributes not only as a reference position to build optimal occlusion in artificial dentition, but is also related to sound periodontal health and stomatognathic function.”7 Visualizing the ideal function can be done using models to better understand the structure necessary to achieve the function and the likely compromises to suboptimal. (Figures 6-7) Once the ideal esthetics and function have been visualized, a key to restoring most patients, but especially patients wearing a MAD, is to involve the interdisciplinary team when discussing the ideal structure and supporting biology, to better understand the possible shortcomings due to the compromise of wearing the appliance, and maybe more important, options for carefully and predictably phasing the treatment. (Figure 8)
Interdisciplinary Communication
Teeth may drift, treatment might need to be phased, or the occlusion might be compromised, all of which and more would benefit from intentional interaction with our specialists. A recent article says it well: “The physiologic tooth position is determined by interactions between the periodontal tissue and occlusal, tongue, and lip forces,” which seems suspiciously familiar to conditions related to airway. It continues to illustrate that often a force or condition (like wearing an appliance that pulls the mandible forward every night), “disturbs the equilibrium of these interactive balances, leading to pathologic tooth migration, often requiring multidisciplinary treatment approaches,” and reinforces the benefit of, “a systematic periodontal-orthodontic-prosthetic treatment for achieving the optimal structural, functional, and esthetic outcomes.”8
 A recent case study involving a patient with severe attrition, again like what we see in patients with airway and sleep issues, reinforces, “how a stable occlusion can be obtained inexpensively. The result of segmented treatment remained optimal and esthetic,”9 demonstrating once more the benefit of not only visualizing the optimal final result, but also including specialists in the process, creating an option for the patient to be ideally restored, regardless of time, money, or dental compromises.
A recent case study involving a patient with severe attrition, again like what we see in patients with airway and sleep issues, reinforces, “how a stable occlusion can be obtained inexpensively. The result of segmented treatment remained optimal and esthetic,”9 demonstrating once more the benefit of not only visualizing the optimal final result, but also including specialists in the process, creating an option for the patient to be ideally restored, regardless of time, money, or dental compromises.
Appropriate Treatment
When the dentist has a clear vision and holds what is possible for the patient as a legitimate option, conversations change and treatment becomes more predictable, fun, and appropriate. The esthetic outcome is visualized, the functional outcome is founded on sound principles, the structure (restorative material, including enamel) is clear, especially with respect to longevity and phasing, and the biology to support the structure, including possible compromises, is clear. Finally, the condition and treatment of the airway is understood, also including any compromises it will have on any of or all four other categories.
A recent article describes how, “Direct resin composite restorations made with the stamp technique are a valuable treatment option for restoring erosively worn dentitions,”10 illustrating that a systematic approach, involving the interdisciplinary team, allows the dentist to better identify what material makes most sense to restore patients, even patients who are wearing mandibular advancement devices.
A patient wearing a MAD can certainly be restored to an optimal esthetic and functional stomatognathic environment. (Figure 9-10) Moreover, understanding the compromise that the appliance brings to the system and the ideal restorative plan, steps can be taken to maintain, as much as possible, the appropriate result, with respect to the esthetics, function, structure and biology for that patient. The best and most appropriate way to “help our patient get worse at the slowest possible rate,” while supporting the “restored” patient, as opposed to the “repair as things break down” mentality might be as simple as a morning deprogramming appliance to remind the body where to go and reinforce a more physiologic and stable environment. (Figures 11-12) Even a patient who is sending the entire stomatognathic system into a frenzy every night by wearing a MAD deserves the option to be optimally restored in a predictable manner, while all parties involved understand the compromises until the root cause is addressed and corrected.