Importance of better screening, more efficient clinical workflow and patient selection in dental sleep medicine
Today, according to the American Academy of Sleep Medicine, about 30 million patients suffer from Obstructive Sleep Apnea (OSA) in the US alone. And unfortunately, about 80% of these patients remain undiagnosed, despite all the efforts and advancements in raising awareness, screening, diagnostic technology and clinical guidelines. The cost associated with this group alone is around 150 billion dollars per year; if we add the cost of treatment it adds up to 162 billion dollars per year. As of today, common treatment options are Continuous Positive Airway Pressure (CPAP), Oral Appliance Therapy (OAT) and surgical interventions, in combination with lifestyle modifications. The most common prescribed treatment remains to be CPAP at 85%, despite its not so impressive long-term compliance rate. Per the same study, only 60% of patients on CPAP remain adherent to this therapy, while the other 40% choose to discontinue treatment for various reasons. While the compliance rate and patient acceptance with OAT seems to be higher, the utilization rate remains very low at 5-10%, despite its proven efficacy in 50-60% of all patients. Closer scrutiny of the numbers reveals that our current model is resulting in about 40% inefficiency; i.e. 40% of patients that are prescribed CPAP are not using it and about 40% of all OSA patients that are OAT responders do not receive the care they need.
Keeping all the above in mind, we seem to have a big problem on our hands and our current models do not seem to be providing adequate solutions.
 A popular justification that has grown over the last few years is to rationalize the poor OAT efficacy in non-responders by higher compliance rate. Although in some patients this might be true, generalizing this to all patients and setting our protocols based on that could prove to be an inefficient approach long-term. In my opinion, that is to “set the bar low”, to pass, as opposed to “raising the bar” by better treatment protocols and approaches. It is like saying; “OAT may not be better than CPAP, but it’s not worse either” and use this justification to increase utilization!!! In this era, when the health industry is working more and more towards precision medicine, this approach seems to be a bit backwards and perpetuates a “trial and error” model. Looking up the definition of “Precision Medicine” online, it is described as a “medical model that proposes the customization of healthcare, with medical decisions, practices, and/or products being tailored to the individual patient. In this model, diagnostic testing is often employed for selecting appropriate and optimal therapies based on the context of a patient’s genetic content or other molecular or cellular analysis.” Also, “Precision Medicine” refers to the tailoring of medical treatment to the individual characteristics of each patient. It does not literally mean the creation of drugs or medical devices that are unique to a patient, but rather the ability to classify individuals into subpopulations that differ in their susceptibility to a disease, in the biology and/or prognosis of those diseases they may develop, or in their response to a specific treatment. Preventive or therapeutic interventions can then be concentrated on those who will benefit, sparing expense and side effects for those who will not.”
A popular justification that has grown over the last few years is to rationalize the poor OAT efficacy in non-responders by higher compliance rate. Although in some patients this might be true, generalizing this to all patients and setting our protocols based on that could prove to be an inefficient approach long-term. In my opinion, that is to “set the bar low”, to pass, as opposed to “raising the bar” by better treatment protocols and approaches. It is like saying; “OAT may not be better than CPAP, but it’s not worse either” and use this justification to increase utilization!!! In this era, when the health industry is working more and more towards precision medicine, this approach seems to be a bit backwards and perpetuates a “trial and error” model. Looking up the definition of “Precision Medicine” online, it is described as a “medical model that proposes the customization of healthcare, with medical decisions, practices, and/or products being tailored to the individual patient. In this model, diagnostic testing is often employed for selecting appropriate and optimal therapies based on the context of a patient’s genetic content or other molecular or cellular analysis.” Also, “Precision Medicine” refers to the tailoring of medical treatment to the individual characteristics of each patient. It does not literally mean the creation of drugs or medical devices that are unique to a patient, but rather the ability to classify individuals into subpopulations that differ in their susceptibility to a disease, in the biology and/or prognosis of those diseases they may develop, or in their response to a specific treatment. Preventive or therapeutic interventions can then be concentrated on those who will benefit, sparing expense and side effects for those who will not.”
In his 2015 State of the Union address, U.S. President Barack Obama stated his intention to fund a United States national “precision medicine initiative”. The Mission Statement of the Precision Medicine Initiative reads: To enable a new era of medicine through research, technology, and policies that empower patients, researchers, and providers to work together toward development of individualized treatments. This is a powerful statement of our mission in treating OSA; we need to reflect on how we can apply new technologies in order to achieve this goal of individualized treatments.
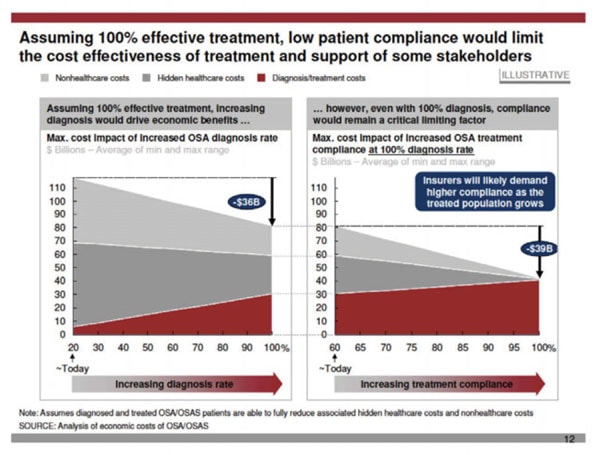
 Another approach would be to say that OAT should be prescribed in the 40% CPAP non-compliant population as an alternative. At first, this may look like a great idea. However, the reality is different and we cannot ignore that only 50-60% of these patients will fully respond to OAT and in the other 40% the OSA will remain uncontrolled. This adds cost to the system both indirect associated with untreated disease and direct, associated with inefficient clinical models (e.g. the cost of OAT in a non-responder). It is estimated that the cost associated with diagnosis and treatment of OSA in the US alone was around ~4.7 billion dollars in 2015. Keeping that cost in mind, it would be easy to see how any small inefficiencies in the model could result in hundreds of millions of wasted dollars. According to a report published by Harvard School of Medicine, assuming 100% treatment effectiveness, increasing diagnosis would drive economic benefits. Even with 100% diagnosis, compliance will remain a critical limiting factor and insurers will likely demand higher compliance as the treated population grows, and perhaps push more towards “Precision Medicine” to improve efficiencies.
Another approach would be to say that OAT should be prescribed in the 40% CPAP non-compliant population as an alternative. At first, this may look like a great idea. However, the reality is different and we cannot ignore that only 50-60% of these patients will fully respond to OAT and in the other 40% the OSA will remain uncontrolled. This adds cost to the system both indirect associated with untreated disease and direct, associated with inefficient clinical models (e.g. the cost of OAT in a non-responder). It is estimated that the cost associated with diagnosis and treatment of OSA in the US alone was around ~4.7 billion dollars in 2015. Keeping that cost in mind, it would be easy to see how any small inefficiencies in the model could result in hundreds of millions of wasted dollars. According to a report published by Harvard School of Medicine, assuming 100% treatment effectiveness, increasing diagnosis would drive economic benefits. Even with 100% diagnosis, compliance will remain a critical limiting factor and insurers will likely demand higher compliance as the treated population grows, and perhaps push more towards “Precision Medicine” to improve efficiencies.
So, how can we move Dental Sleep Medicine in the same direction?
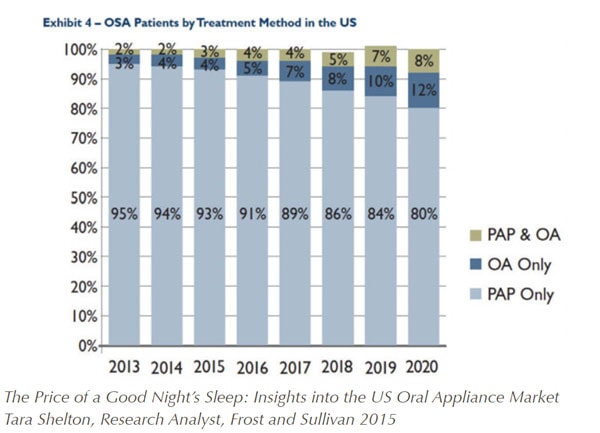
Per the Frost and Sullivan Report, the US market will grow from 180,000-200,000 patients fitted with a custom made oral appliance in 2013 to over 1,000,000 patients in 2023. Although this may sound very promising and a step in the right direction, it does not necessarily associate with better utilization of OAT as an alternative treatment for OSA patients. As seen in the figure below, the percentage of patients utilizing OAT will remain quite low at ~12% by 2020.
As well, we must consider the cost associated with the OAT non-responders in this small group. According to the AASM in 2016, the cost associated with undiagnosed/untreated OSA is around $6336 per patient. Using this number and the direct cost associated with OAT (Average: $2,000) and the estimated 1,000,000 patients treated with OAT, the total cost associated with OAT non-responders is easily estimated. Although the anecdotal clinical non-responder rate differs from one practitioner to another (e.g. depending on the level of expertise, tools and technologies utilized, treatment philosophy,…), I decided to use a conservative 20% non-responder rate. This will result in 200,000 ineffective OAT per year, which will in turn result in ~1.7 billion dollars per year of wasted money in Dental Sleep Medicine (200,000 x (Cost of untreated disease: $6336.00 + Cost of OAT: $2000). That is in fact the cost associated with a “trial & error” method as opposed to a precision medicine model.
On a smaller scale and focusing on individual patients and dental sleep practices, some of the direct and indirect costs associated with treatment of OAT non-responders could be:
Cost to the patient:
- Monetary cost associated with the therapy
- Cost of reparative therapy if OAT was abandoned due to physical complications
- Adverse health consequences associated with untreated OSA
- Potential loss of confidence in the system and alternative therapies
Cost to the Dentist:
- Cost associated with the lost chairtime (It is commonly believed that OAT non-responders require an average 4-6 additional appointments compared to OAT responders, due to difficulties/challenges associated with their treatment process)
- Indirect cost associated with patients’ loss of confidence in the dentist and perhaps leaving the clinic
- Indirect cost associated with the referring healthcare professionals’ loss of confidence in OAT and the dentist, reducing referrals for OAT.
- Indirect cost of loss of confidence within the dental team, reducing screening activities and growth of SDB treatments by the dental practice.
Aside from the health economics of Dental Sleep Medicine, there are many other challenges that we’re facing today, such as high number of undiagnosed patients.
This is a challenge that is not specific to dentists, but to Sleep Medicine in general.
Dentists can play a major role in helping with this area, as they can screen many patients that are currently in their practices. An average dentist has between 1500-2000 active patients which they see once or twice per year and have about an hour during their hygiene appointments to discuss various topics including OSA. However, today less than one third of dentists screen for OSA and even in those clinics the screening seems to be inconsistent.
 Over the years I’ve had the privilege of helping, meeting and training many dentists in Dental Sleep Medicine across the world and tried to keep in touch with most of them, if possible. Despite all the initial excitement, continued effort and commitment to implementing OAT in their clinics, the majority of the offices fail to keep up the sleep program over the years. When looked deeper into this loss of interest, the barriers seems to remain the same for most clinics, despite all their other differences. Aside from general challenges to implementation of any new program in a dental clinic (the need for proper training, team training, consistency and daily huddles, time and many other factors) there seem to be specific issues that are related to Dental Sleep Medicine:
Over the years I’ve had the privilege of helping, meeting and training many dentists in Dental Sleep Medicine across the world and tried to keep in touch with most of them, if possible. Despite all the initial excitement, continued effort and commitment to implementing OAT in their clinics, the majority of the offices fail to keep up the sleep program over the years. When looked deeper into this loss of interest, the barriers seems to remain the same for most clinics, despite all their other differences. Aside from general challenges to implementation of any new program in a dental clinic (the need for proper training, team training, consistency and daily huddles, time and many other factors) there seem to be specific issues that are related to Dental Sleep Medicine:
- Difficulty in referring patients to sleep physicians for proper testing and diagnosis, resulting in long waitlists, financial and time cost. Many patients lose interest and become lost to the system.
- From the patients that make it to the diagnostic phase, only 5-10% are referred to the dentist for OAT and the rest are prescribed CPAP. Out of the 5-10% OAT referrals, many have already tried CPAP, for many reasons were either non-compliant or did not experience the immediate benefits, and become hesitant or lack confidence to start a new treatment.
- From the ones are still interested in OAT, the consultation seems to be a bit of a challenge. When asked if the OAT will work for them and how, most dentist seem to have a problem with telling the patients that it may or may not work for them and the only way to know is to make an appliance and go through the subjective titration protocol and commit to the time and financials costs.
- The same issue also seems to pose a challenge for dentists that are trying to have a dialogue with sleep physicians and other healthcare professionals about OAT and raising awareness. They seem to hit a roadblock when asked the same question: “Is this going to work and how long before efficacious treatment is achieved?” Although research has shown many benefits of OAT and also novel ways of looking at treatment effectiveness (such as Mean Disease Alleviation) have given dentists tools to be better equipped for such discussions, the reality is most prescribers consider OAT a secondary treatment option in CPAP non-compliant patients, as opposed to an equal treatment alternative in the OAT responders.
- In patient consultation, as dentists we are trained to provide the best evidence-based treatment for our patients with good to excellent prognosis. Every day, we’re using better diagnostic tools and material to improve the quality of general dental care and minimize the uncertainty. However, in Dental Sleep Medicine (DSM) we’re faced with a big challenge of accepting 60-80% rate of success (depending on clinician’s experience and how “liberal” they are with patient selection) and a “trial and error” method. Such uncertainties reflect on the dentist during the consultation appointment and does not convey the level of confidence that many patients require from their treating clinician and consequently their final decision on whether to go ahead with treatment.
Despite all the challenges above, some dentists remain motivated to help patients and will continue their efforts for a while. However, after a while, like any other added service in a dental practice, the financial realities of running a business will kick in. If only 5-10% of diagnosed patients are referred to a dentist for OAT, the ratio of number of patients screened to the number of patients that invest in OAT will remain very low, perhaps around 3-5%. That means for every 100 patients screened for OAT, the dentist may end up making 5-10 appliances in our current model. If we were to look at this solely from a “Return on Time Invested” point of view and time spent on screening and referrals for 100 patients to only get 5-10 appliances, the results won’t be very impressive long-term, especially when compared to other dental procedures in a clinic. To make things even more challenging, out of the 5-10 appliances fabricated, without objective patient selection, there will be a few non-responders that will cost the dentist excessive chairtime, loss of patients’ trust and referring physicians’ trust. These daunting challenges make many dentists think twice about providing such services in their clinics long-term, despite all the potential values and ethical obligations. Too many patients will be left undiagnosed or untreated. And as discussed earlier, to create any meaningful impact on this epidemic, the sleep field and patient population require as much help as possible. Losing dentists that are interested in providing OAT is doing the exact opposite.
So, what’s the solution and do we have the necessary tools?
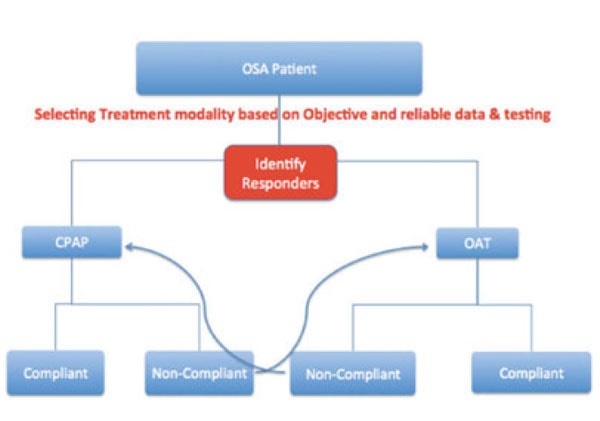
As the medical model focuses more on “precision medicine”, dentistry has no choice other than to follow and we need to move away from segregation between the two professions and become more united. We require a new approach, new model, new clinical guidelines. A model in which the patient is offered their therapeutic choices and asked their preference, and before proceeding with such treatment, the efficacy of such potential treatment can be prospectively tested. This will allow the patients to receive the therapy of their choice, with confidence in the therapeutic outcome. Individualized care and patient selection will become key factors in such model.
 This could also result in an improved cost-to-benefit ratio in the system, by avoiding the costs associated with inefficiencies discussed earlier.
This could also result in an improved cost-to-benefit ratio in the system, by avoiding the costs associated with inefficiencies discussed earlier.
This “Test, Select, Treat” model could perhaps be a novel, yet very effective approach in our battle against the epidemic. Although there have been many studies on utilizing different techniques and technologies for patient selection for OAT, such as Cephalometric Characteristics, 3D/CBCT Imaging, acoustic imaging, CPAP pressure, Mallampati score & BMI, as of today the actual role of such techniques remains unclear in the clinical practice due to low Positive Predictive Value (PPV) or Negative Predictive Value (NPV). However, there are promising approaches such as RCMP (Remotely Controlled Mandibular Titration – MATRx), UACP Multisensor Catheter and DISE (Drug Induced Sleep Endoscopy) that have better PPV & NPV that could be useful in clinical practice.
As the only prospectively validated and commercially available technology for patient selection for OAT, MATRx would allow the physician to select responders to OAT AND to also provide a target protrusive position at which an efficacious treatment can be achieved, minimizing the chairtime required for treatment and the number of non-responders. MATRx has now been available in North America for a few years and recently, to further simplify the workflow and increase accuracy and efficiency of OAT, an “At-Home” version, MATRx Plus, has been developed and shows predictive accuracy comparable to that of its parent, MATRx. MATRx plus is commercially available in Canada and is in beta testing in the US. From DSM perspective, being able to accurately and confidently identify OAT responders, prior to initiation of OAT, could have many positive impacts that go beyond just selecting patients. By being able to identify OAT responders after initial OSA diagnosis, dentists could see an increase in referrals for OAT, perhaps as high as 50-60% of total patients diagnosed, as opposed to the current 5-10%. Not only the number of referrals would increase, the dentists will be minimizing the number of OAT non-responders, essentially eliminating the costs associated with this group of patients. This could change the nature of consultation with patients as the two unknown factors that currently complicate the process (i.e. whether the appliance will work AND where to set the mandible/calibration) will be eliminated, giving both the dentist and the patient more confidence in therapy. This could also result in improved treatment acceptance by patients during consultation.
Another very important advantage would be the ability to have a confident and evidence-based dialogue with referring physicians, and giving them confidence in recommending OAT as the first line of treatment.
With the increased number of referrals, higher treatment acceptance, minimized (perhaps eliminated) OAT non-responders, less chair time required for achieving efficacious treatment (because of the known target protrusion) and avoidance of subjective calibration, the economics of DSM could improve significantly, making it more appealing to a higher number of dentists. With more dentists involved and more screening, we can make a meaningful impact on the OSA epidemic and move in the right direction: Precision Medicine.
What’s next as we see more and more patients?
No individual technology or advancement in the field is going to magically resolve all the existing problems. This reminds me of a documentary that I watched a while ago on the Second Industrial Revolution; “Between 1860-1900, many new technologies, including electric power, were put to use. These inventions launched a transition to a new economy, a period of about 70 years of ongoing, rapid technical change. After this revolution began, however, several decades passed before measured productivity growth increased. This delay is paradoxical from the point of view of the standard growth model. Historians hypothesize that this delay was due to the slow diffusion of new technologies among manufacturing plants together with the ongoing learning in plants after the new technologies had been adopted. The slow diffusion is thought to be due to manufacturers’ reluctance to abandon their accumulated expertise with old technologies, which were embodied in the design of existing plants and trying to fit the new technology into their existing work-flow models and set their production goals based on their current resources and models. In fact they needed to do the opposite: Designing the Workflow and Protocols based on the “Final Goal” & “Available Resources & Technologies.” Perhaps DSM needs the same approach and thinking outside the box.
 With increased demand for OAT, DSM requires:
With increased demand for OAT, DSM requires:
- Better patient selection
- Avoidance of Non-responders
- More efficient workflow
- Less chair-time
- “Target” Oriented models
- Avoidance of Failures
- Improved Clinical Protocols and Techniques
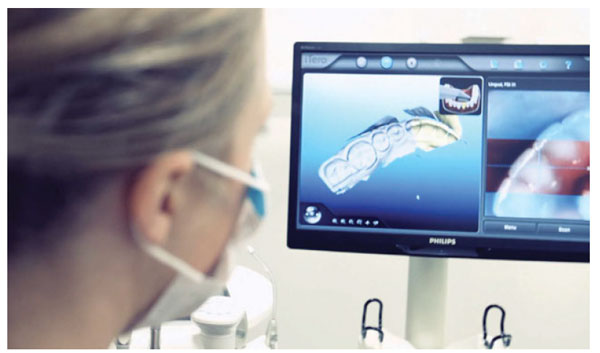
- Digital Workflow
- Better chair-side techniques
- Better “bite registration techniques”
- Better Guidelines (Evidence-Based)
- That cannot be easily challenged by other industries
- More Efficient Device Manufacturing
An exciting journey ahead!!!
