CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims
The purpose of this article is to review the tools helpful in evaluating and treating OSA – with a special emphasis on intraoral scanning.
Expected outcomes
Dental Sleep Practice subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader will:
- Understand intraoral scanners’ role in patient education.
- Realize intraoral scanners’ role in practice documentation.
- Appreciate intraoral scanners’ impact on the fit of final appliances.
- Recognize the impact of open source digital files on practice workflow in appliance fabrication.
The Tools that Make a Difference for the Practitioner and the Patient
by Stephen D. Poss, DDS
Introduction
When the American Dental Association released a policy in October 2017 that encouraged dental professionals to screen for obstructive sleep apnea (OSA) and other sleep-related breathing disorders (SRBD)1, it created a dramatic shift in the role dentists play in SRBD treatment. In addition, the public’s awareness of the comorbidities associated with OSA – high blood pressure, diabetes, gastric reflux, weight gain, atrial fibrillation, heart attacks and increased likelihood of cancer2,3 – has increased significantly in recent years, and patients have begun to seek solutions from their dentists. Technological advancements related to this issue are helping doctors evaluate and treat OSA more efficiently and effectively than in the past. As a result, practitioners who focus on sleep medicine are increasingly using 3D imaging systems along with intraoral scanners and cameras to not only facilitate their OSA evaluation and treatment, but also to educate their patients on their treatment options.
Evaluating for OSA
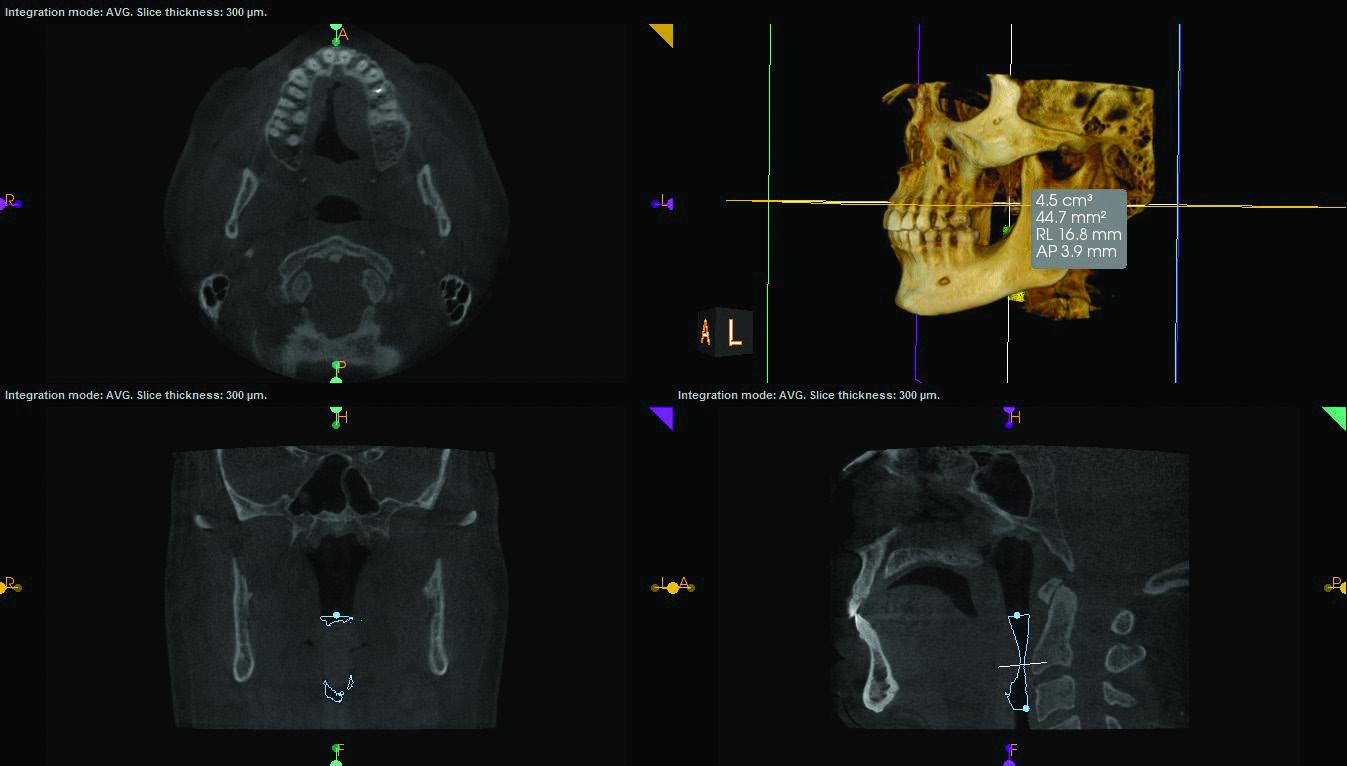
When I am evaluating a patient for OSA, I look at the same things insurance companies want verification of: sound dentition (usually a minimum of seven teeth on each arch); temporomandibular joint (TMJ) health; no active decay; and the periodontal status of the patient. I could choose to take a full series of X-rays to accomplish this, which would result in approximately 24 films and significant radiation. However, a cone beam computed tomography (CBCT) system with a large field of view, like Carestream Dental’s CS 9300, enables me to capture the entire airway space – including the teeth and TMJ – all on one film. The large field of view helps me identify preexisting conditions, including current joint positioning. This information is important to collect not only for the evaluation, but also for documentation purposes.
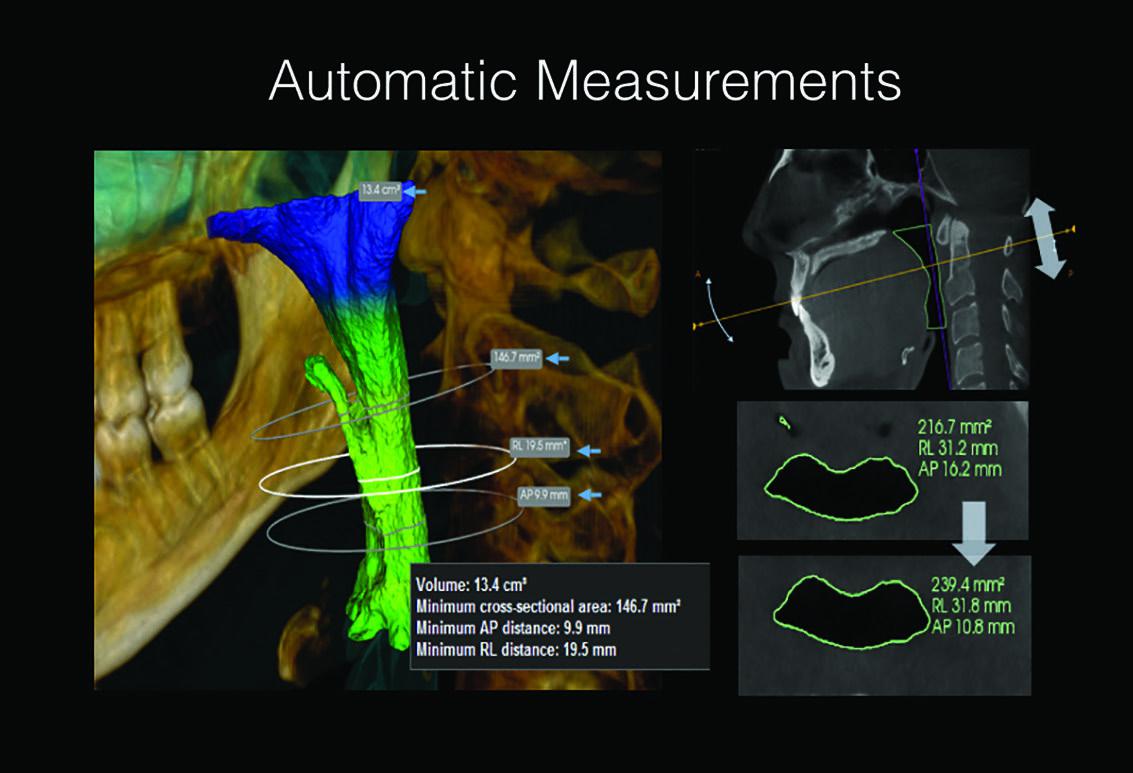
Most obstructions are in the uppermost part of the airway, which is the velopharyngeal region.4 Mandibular advancement devices cause forward displacement of the mandible and prevent oropharyngeal airway obstruction indirectly by moving the suprahyoid and genioglossal muscles anteriorly. It was also suggested that forward and inferior displacement of the mandible decreases the gravitational effect of the tongue in the supine position and enlarges the velopharynx by stretching the palatoglossal and the patatopharyngeal arches.5
Intuitively, one would think that mandibular advancement should improve the sagittal dimension of the oropharynx. However recent studies suggest that increases in the upper-airway caliber occur in the transverse dimension at the level of the velopharynx.6 Others indicate that the changes occur in the sagittal dimension and cross sectional area. Hence the anatomic changes induced by mandibular advancement appear to be quite complex. This could be due to the intricate linkages between upper-airway structures.
There are studies supporting that the further down the pharynx the obstruction is occurring does make it more difficult to treat with a mandibular advancement device. This is especially true if the obstruction is more in the area of the hypopharynx.7
This is not to say a CPAP intolerant patient with a constriction in the hypopharynx could not be treated. A study done by Allan Lowe in 15 patients demonstrated that the hypopharynx did increase in cross sectional area by 18%.8
Typically I have found several factors that can influence my thoughts on the success of an oral appliance therapy. Age and BMI and the severity of the AHI are the most obvious. The clarity of the nasal passages as well as locating the narrowing of the airway space in the pharynx is also helpful in determine a successful outcome.
CBCT technology is not for diagnosing OSA but it can assist the clinician trying to meet the expectations of the patient. CBCT along with an intraoral scanner can help determine the appropriate appliance that will best accomplish my treatment goals.
Presenting the Case

Intraoral scanner imaging assists me in educating the patient and setting treatment expectations. I can merge the files from the CBCT system and the intraoral scanner, providing a comprehensive view of the patient’s clinical situation. If, for example, the airway constriction is lower in the airway, I can present the case with images that make it easier for the patient to understand why an appliance may not improve his or her OSA completely. By contrast, if I feel confident that a 70 to 80 percent improvement is more likely, then the patient has the visual information to help him or her determine if treatment is worth pursuing.
Another useful tool in case presentation is the intraoral camera, which can capture the tongue, tonsils and uvula. These photos can be very helpful in communicating the potential effectiveness of OSA treatment. For example, Figure 1 shows the high, enlarged tongue and narrow airway space, which would be considerably smaller when the patient is lying down.9 Figures 2, 3 and 4 are CBCT images that provide additional information about the patient. Together with his sleep test diagnosis of severe OSA (AHI 54), these images indicate that the patient’s clinical situation may be difficult to treat. Images such as these can enable the patient to make a more informed decision about treatment options.
Fitting the appliance
Once the appliance is fabricated, I fit the appliance to the patient. The accuracy of the intraoral scanner has a direct impact on the fit of the appliance: the greater the accuracy of a digital impression, the better the fit of the appliance, which allows for quicker seating and reduced chair time.
Replacing the appliance
The reasons for which a patient might need a replacement appliance are many. Loss is one – a patient might leave the appliance behind in a hotel room, for example, and cannot easily return to retrieve it. Wear and tear is another reason. Over time, an appliance can become worn and ill fitting, requiring the fabrication of a replacement. Damage is yet another reason, and the family pet is very often the culprit. Pets find appliances especially enticing, even when the greatest care has been taken to prevent access.
Thanks to digital models, I can set the wheels in motion to fabricate a replacement – for any of these reasons – with just a few clicks in the software. The process can be very fast if the intraoral scanner has an open system. I can send the open source digital files from Carestream Dental’s CS 3600 intraoral scanner, for example, to the lab electronically and request a reprint of a patient’s device. The STL files arrive at the lab in minutes – and without issue of compatibility – enabling the lab to work in the design software of its choice. Patients do not have to experience the inconvenience of making a special trip to the practice and the delay in fabrication that this step causes. For many patients, the idea of spending several nights without an appliance – which has mitigated their symptoms and upon which they’ve grown reliant – can cause distress and anxiety. Consequently, the faster the replacement can be made, the sooner patients can resume sleeping at the level they’ve grown accustomed to with OSA therapy.
A side effect of oral appliance therapy is that a patient’s teeth can move. As a result, a patient’s jaw can reposition.10 Digital models are beneficial in terms of documentation, for both the patient and the practitioner. With the visual evidence, the patient can more easily understand her clinical situation before and after OSA therapy; and the practitioner has an original reference to access if a question arises in the future.

Preventing the need for a new appliance
Digital models can also prevent the need to replace an appliance. When clinical situations change due to broken teeth, cavities, implants, etc., I can provide guidance to the general practitioner and the lab on the fabrication of the restoration. An over-contoured crown, for example, may cause the oral device to no longer fit. For the existing device to continue to work, the new restoration must be the same size and shape of the original tooth. I can share images with the patient’s dentist and even print a model for the lab to use to ensure the oral device is still functional with the new restoration.
Conclusion
As sleep disorders – and information about them – become more prevalent among the population, dental professionals will have an important role to play in treating them. Through the use of technology, practitioners will be better able to understand potential treatment options and to present them to their patients. The benefits of using CBCT imaging, intraoral scanners and intraoral cameras are multiple; improved appliance fit, better documentation and enhanced communication are all advantages. But perhaps the biggest benefit of all is having the opportunity to improve patients’ sleep along with their overall health and quality of life.
References
1. https://www.ada.org/en/press-room/news-releases/2017-archives/october/ada-adopts-policy-on-dentistry-role-in-treating-obstructive-sleep-apnea.
2. https://well.blogs.nytimes.com/2012/05/20/sleep-apnea-tied-to-increased-cancer-risk/?ref=health.
3. Calvin, A.D., Albuquerque, F.N., Lopez-Jimenez, F., Somers, V.K., “Obstructive Sleep Apnea, Inflammation and the Metabolic Syndrome,” Metab Syndr Relat Disord, 2009 Aug: 7 (4): 271-277.
4. Ferguson, Kathleen, “Oral Appliances for Snoring and Obstructive Sleep Apnea,” Sleep, 2006, Vol. 29, No. 2, 245-262.
5. Three-dimensional computer-assisted study model analysis of long term oral appliance wear. Alan Lowe, Fernanda de Almeida: American Journal of Orthodontics and Dentofacial Orthopedics September 2008 393-416
6. Three-dimensional upper-airway changes associated with various amounts of mandibular advancement in awake apnea patients. Xiaoguang Zhao, Yuehua Liu; Am J Orthod Dentofacial Orthop 2008; 133:661-8
7. Effects of an anteriorly titrated mandibular position on awake airway and obstructive sleep apnea severity. Satoro Tsuiki, DDS PhD, Alan Lowe, DMD, Fernanda Almeida DDS American Journal of orthodontics and Dentofacial Orthopedics May 2004 548-554
8. Mandibular advancement oral appliance therapy for obstructive sleep apnoea: effect on awake caliber of the velopharynx. C F Ryan, LL Love Thorax 1999; 54; 972-977
9. Cartwright, Rosalind, “Sleep Position Training as a Treatment for Sleep Apnea Syndrome,” Sleep, 1985, Vol. 8, (2), 87-94.
10. Hui, Chen, Lowe, Alan, “Three-Dimensions Computer-Assisted Study Model Analysis of Long-Term Oral Appliance Wear,” American Association of Orthodontics, 10.2006.10.030.
 A graduate from the University of Tennessee College of Dentistry, Stephen D. Poss, DDS, lectures internationally on esthetic dentistry, sleep apnea and TMD. He is a Diplomate with the ABCDSM, ACSDD in dental sleep medicine and a Fellow with the American Academy of Craniofacial Pain. Dr. Poss is an active consultant to several dental manufacturers for new product development and refinement. He has had numerous articles published in most of the leading dental journals. Dr. Poss maintains a restorative and TMD practice in Brentwood, Tennessee. He can be reached at
A graduate from the University of Tennessee College of Dentistry, Stephen D. Poss, DDS, lectures internationally on esthetic dentistry, sleep apnea and TMD. He is a Diplomate with the ABCDSM, ACSDD in dental sleep medicine and a Fellow with the American Academy of Craniofacial Pain. Dr. Poss is an active consultant to several dental manufacturers for new product development and refinement. He has had numerous articles published in most of the leading dental journals. Dr. Poss maintains a restorative and TMD practice in Brentwood, Tennessee. He can be reached at