CE Expiration Date: May 7, 2021
CEU (Continuing Education Unit):1 Credit(s)
AGD Code: 730
Educational objective
Dental Sleep Practice subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will exhibit the reader understands:
The reason for publishing this case report is to underscore the need for the dentist to be aware of multiple problems presenting in one patient will demand vigilance in documentation and observation of symptoms. One problem might seem paramount, but the clinician must keep asking questions until the true extent of the patient’s condition is discovered. In this case, a surprising result prompted inquiry by the treating dentist, adding to his clinical expertise and prompting further questions. Curiosity in clinical practice will yield more complete patient care. This report was compiled in the hopes of stimulating similar curiosity in the reader-clinician.
by Daniel E. Taché, DMD
And if tonight, my soul may find her peace in sleep, and sink in good oblivion, and in the morning wake like a new-opened flower, then I have been dipped again in God and new-created.
–D.H. Lawrence
Why Publish This Case Report?
My decision to publish the outcome of this one TMD case was threefold:
1. Hypothesis: Epilepsy can be solely a comorbid condition of undiagnosed/untreated sleep-related breathing disorder and that an intraoral airway device can greatly enhance efficacy of treatment when anti-epileptic drugs (AEDs) are insufficient.
It had never occurred to me that I would publish this case report because it started out as do many we treat in our TMD & Sleep-Related Breathing Disorders (SRBDs) limited practice. I begin each case expecting a positive outcome; the result in this case turned out to be surprising and challenging.
This case report concerns a 34 y.o. woman who came to us complaining of severe jaw pain upon awakening and “teeth grinding.” As she accepted and cooperated with our treatment plan, she was progressing well and reported a significant decline in her daily pain. She reported that she was grinding her teeth less. Everything changed approximately 15 months after we had initiated treatment when, in the same week, I was paid a visit by her (adopted) mother and received a phone call from her neurologist of nearly 24 years. They informed me that EJ had has a surprising change in her medical status. I had known since the comprehensive examination and what I thought was an exhaustive Past Medical History (PMH) 15 months earlier that my patient, EJ, had been diagnosed with epilepsy at the age of 10. As you’ll see, her report was shallow, I was focused on the immediate problem, and I knew little about any connection between epilepsy and TMD or SRBD. Briefly, none of her treatment had resolved the epilepsy and she continued to have seizures weekly for all of those years. What I learned that week was that since the first night that she wore the intraoral device we provided for her TMD, she had not had a single seizure! This happy result continues to this day.
Naturally, I was compelled to learn more about epilepsy. I was most interested in the possible correlation between undiagnosed SRBDs and epilepsy because the intraoral device that we provided did address the intra-articular (TMJ disc displacement) component of her TMD problem but it also addressed her sleep-related bruxism, because I hypothesized that it augmented what did appear to me to be a problem of sleep fragmentation due to airway instability/collapse while sleeping.
What I found after I began to review the epilepsy literature was confusing when considered in the context of this case. The general views regarding the epilepsy/SRBD relation was that “excessive daytime sleepiness is a common complaint of epileptics” (Piperidou, 2008), “examples of sleep-related disturbed behaviors (parasomnias) are epilepsy or asthma” (Stores, 2007), “patients suffering with epilepsy frequently complain of unrefreshed sleep” and “the prevalence rate of OSA can be very high” (Malow, 2000). In spite of the significant amount of evidence which strongly suggests a bi-directional correlation between epilepsy and OSA, most authors portray the issue of sleep disturbances as merely a comorbidity rather than an isolated medical condition that is actually provoking the epileptic seizures.
One article struggled to explain the possible correlation by hypothesizing that “antiepileptic drugs (AED) influence OSA as can barbiturates and benzodiazepines,” and “weight gain in patients treated with valproate, may precipitate or exacerbate OSA.” It seemed to me that the authors of so many articles could not allow themselves to conclude at any point that epilepsy may solely be a comorbidity of OSA and that merely identifying and treating the OSA might be sufficient.
My literature review proved to be very frustrating when considered in the light of EJ’s outcome. Further review surprisingly revealed a possible explanation for this thought-process shortcoming: deficiencies in the training of healthcare professionals. As long as conventional history-taking fails to include evidence-based sleep screening tools for SRBD it is unlikely that sleep disorders will be correctly identified.
Surveys of medical schools curricula have revealed that out of a typical 5 year undergraduate course of study, the median time spent on formal teaching about sleep and consequent comorbid diseases ranges from 5 minutes – 2 hours! (Stores, 2007) (Stores, 2009)
After talking with EJ’s neurologist, I was confident that our hypothesis was confirmed: that her TMJ dysfunction is largely a comorbidity of sleep fragmentation, mostly shown by her sleep-related bruxism. This sleep fragmentation has regularly provoked her epileptic seizures for nearly 24 years. My confidence stems from the observation that the epilepsy is now completely controlled by use of an intraoral Mandibular Advancement Device.
So, why did I feel that this case report should be published? “Clinicians can contribute to scientific knowledge significantly in a variety of ways and the Case Report can be an effective means to identify new diseases or (epidemiologically-speaking) the adverse effects of new exposures and new links between an exposure and a disease” (Aschengrau, 2013).
Case reports are certainly lower down on the pyramid of evidence however, they do have a place in advancing scientific knowledge. Case reports can add clarity to cause and effect by creating links between a condition and a clinical manifestation or an outcome of treatment of that “condition” that heretofore, had not caught the attention of others. Quite often, as in the case reported herein, because of bias. The discovery of AIDS and the relationship between breast cancer and ionizing radiation are just two of many diseases that were first mentioned in case reports.
2. Inform: to inform you, the dental clinician, of the inescapable fact that all “… dental patients were found to have a high pretest probability of having undiagnosed OSA,” much higher than that of the normal population. Estimates show a prevalence of 33% of males and nearly 19% of all female dental patients who present for general dental procedures and/or hygiene, to be at high risk for SRBD (Levendowski D. M., 2008).
An equally disconcerting fact is that in a primary care medical setting, the prevalence of patients at risk for SRBDs is similar to that of general dental practice yet, numerous surveys have shown that Primary Care Physicians (PCPs) do not routinely screen patients for OSA (Mold, 2011) (Sorscher, 2008). More specifically these surveys reported both a low rate of recognition and diagnosis of sleep disorders in both outpatient and inpatient health care settings. The range of rates of patients who were both identified and referred for treatment were a dismal 0.1 – 3.1% of all patients (Rosen, 2001) an alarming statistic.

 3. Implore: to implore you to consider the moral or categorical imperative of NOT examining your patients for SRBD in light of the failure of the medical profession to do so and even more so because of the relative ease of identifying dental patients at risk. Even a cursory intraoral & extraoral inspection, coupled with the simplest of evidence-based screening tools, makes identification of patients who should be referred for a sleep study relatively simple, especially when the clinician also has at hand Past Medical and Family history documentation.
3. Implore: to implore you to consider the moral or categorical imperative of NOT examining your patients for SRBD in light of the failure of the medical profession to do so and even more so because of the relative ease of identifying dental patients at risk. Even a cursory intraoral & extraoral inspection, coupled with the simplest of evidence-based screening tools, makes identification of patients who should be referred for a sleep study relatively simple, especially when the clinician also has at hand Past Medical and Family history documentation.
Every medical professional is compelled to identify at-risk patients because undiagnosed/untreated sleep disorders carry an increased risk of developing physical and psychiatric illness, among them notably cardiovascular disease, complications in pregnancy, diabetes, anxiety, depression, and alcohol and other substance abuse.
It is my hope that consideration of this background information, coupled with the clinical case which you are about to consider, that even if you do not intend to actually treat the DSM patient, that you will feel compelled to seek, in a more formal way, seminars/courses regarding DSM so that you will begin to institute a screening program within your practice. You must begin to identify patients at risk for SRBD and make arrangements to refer them to a competent clinician if you have no plans to treat such patients.
Dental sleep medicine is perhaps the most rapidly expanding dental service today. Current evidence (Ramar, 2015) shows that oral airway devices are as effective as nasal CPAP in the treatment of snoring and mild to moderate OSA. Although as dentists we cannot diagnose OSA, it is within the scope of the practice of dentistry to facilitate our patients being identified and referred to qualified sleep specialists. After diagnosis, when appropriate, our DSM services may help a vast majority of these patients.

4. Opportunity: opportunity to treat patients who are seeking your services because their quality of life has been so adversely affected by their untreated SRBD. DSM has added a great deal of meaning to my practice as it has for many because we are treating life-degrading/life-threatening disease and our patients understand this and want your expertise.
As was stated previously, if our dental population has SRDB as high as 33% male and 19% female, your patients who complain of “grinding” and have TMD signs and symptoms are at high risk of SRBD, with as many as 42-47% with both disorders. (Smith M. W., 2009). The implication is obvious, namely that “clinicians who are treating TMD patients need to be ever vigilant that their patient has a high probability of having an undiagnosed SRBD. You should be screening “all patients for sleep disorders and you should be developing relationships with board certified sleep physicians who will help facilitate getting your patients diagnosed and treated with oral airway devices and/or nasal continuous positive airway pressure devices” (Smith M. W., 2009). This is now the standard of care in dentistry. The bar has been raised and we must all be up to the task.
Table 1 to the left along with the Figure 1 photographs are a fairly comprehensive list of dental signs and symptoms which often present in patients with fragmented sleep. These signs and symptoms of SRBD are encountered by nearly all dentists, both the general and specialist dentist alike daily in their practice of dentistry. Unfortunately, too often these signs and symptoms are viewed by the profession as primary DENTAL COMPLICATIONS, not co-morbid conditions signaling a more ominous condition hence, the symptom is treated, and the patient is released unaware that this medical problem exists which will continue to degrade their health.
Meet EJ
This is a case study of a patient who was referred to our office for treatment of “TMJ” pain. The very favorable outcome was far more than either EJ or we expected and can be attributed to applying knowledge and skills in dental sleep medicine.
Important: remember however, that suspecting a problem is not a diagnosis, only a suspicion. Currently, diagnosing OSA is not within the scope of the practice of dentistry; a diagnosis is reserved for a board-certified sleep medicine specialist.
EJ’s Chief Complaints
- EJ (Figure 2) is a 34-year-old female patient who was referred to our TMJ/OFP clinic by her primary care physician for “TMJ” pain.
- EJ described her Chief Complaints (CC) as:
- bad night sleeping, she grinds her teeth when she is not sleeping well
- she has noticed that when she grinds her teeth, she awakens with jaw pain
- she has teeth pain day and night after a bad night’s sleep,
- when not sleeping well:
- often awakens feeling sweaty
- 3-4 “bathroom breaks” throughout the night
- EJ began to chronicle her very extensive Past Medical History (PMH) but in very general terms because EJ was referred to us for her jaw pain and nocturnal teeth grinding; at the time, there was no suspected correlation between the pain that she often awakened with and her seizures
- EJ told us that she has been diagnosed with epilepsy dating back for “…more than 20 years …” beginning when she was only 10 years old which was when she experienced her first “seizure”. I later learned that pediatric seizures are a fairly common problem and that most often the seizures do not recur and if they do, they typically respond to one of several Anti-Epileptic Drugs (AEDs)
- Important to Note: EJ, at the time of her initial examination, was 34 years old and although she did inform us that she had been diagnosed with epilepsy, she did not provide much more history on the subject other than that she had been taking AEDs for nearly 24 years. Because EJ had significant neurocognitive problems from her condition, she offered a relatively superficial history at the time of her initial exam and it would be more than a year later that we learned the real history of her epilepsy problem.
EJ’s Past Medical History (PMH)
- Figure 3 shows EJ when she was approximately 10 years of age when her seizures began.
- Her very first seizure occurred in 4th grade while standing in line at a water fountain. She lost consciousness completely for “a couple of minutes”
- EJ was seen by a neurologist who prescribed Phenytoin to prevent future seizures
- The seizures became more frequent despite being on the Phenytoin
- It was noted that all of the subsequent events would occur while she was asleep
- Her condition was reclassified from Idiopathic Seizures to Epilepsy
EJ’s Seizure Treatment: Pharmacological
- AEDs are typically quite effective in controlling pediatric seizures and one AED is sufficient in about 60 percent of children.
- It is notable that by the time I met EJ she was taking as many as five (5) drugs concurrently and she still had sporadic seizures.
Seizure Treatment: Neurosurgery
- EJ’s response to the Phenytoin was poor.
- A brain “lesion” was found on a scan and neurosurgery was recommended.
- Surgery was performed, in fact, she had 3 procedures, including a Vagus Nerve Stimulator (VNS).
- VNS typically will reduce seizures by 50% (Elliott, 2011) however, EJ did not realize any benefit.
- EJ’s seizures, up until the point of surgery, had all occurred while she slept. Following neurosurgery, seizures were now occurring both day and night.
Pediatric Seizures/Epilepsy: Background
- Nearly 120,000 children experience a first or newly diagnosed seizure annually.
- Of first-time pediatric seizure victims approximately 45,000 children will experience recurrence of their seizures
- 60% of the time it will not recur for a decade or more (N. Aprahamian, 2014).
- If there are 2 or more recurrent seizures without a proximal cause for the seizures (Speltz, 2014) this condition will then likely be reclassified as epilepsy.
Provoked Seizures: seizures that follow a discrete event such as:
- Trauma
- Hypoglycemia
- High fever
- Provoked seizures rarely recur after the precipitating condition (fever; infection) has been identified
Unprovoked seizures: seizures which do not have an obvious immediate precipitating event. The nature of these seizures suggests the possibility of an underlying neurological disorder or serious medical condition that might predispose a child to recurrent seizures such as:
- Genetic and congenital malformations
- Intrauterine and postnatal insults
- Anoxic injuries
- Infections (viral and bacterial)
- Vascular malformations and compromise (e.g. Ischemia)
- Trauma
- Tumors
- Seizures with unknown etiology


Figure 4: EJ’s Mandibular range of motion and Figure 5: TMJ, sagittal view – open (bottom) and closed (top)
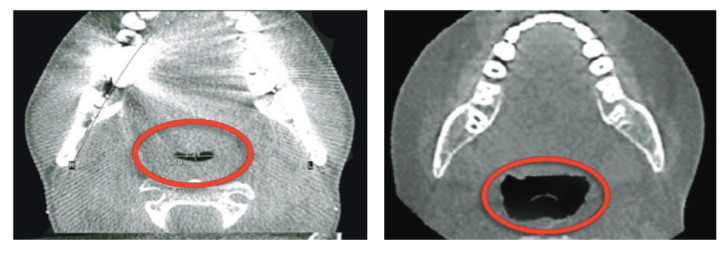
Figures 6A-6B: CBCT image/axial view A. EJ’s airway. B. Normal airway

Figure 7: Radiologists comment
Temporomandibular Joint Clinical Evaluation
- Figures 4 shows the TMD examination.
- Maximum opening (MO) was moderately limited at 35mm
- Lateral movement was normal at 10mm
- Muscle palpation: multiple muscles were tender to palpation most notably a) bilateral superficial masseters, bilateral lateral pterygoids, anterior temporalis, mid-temporalis, and splenius muscles
- External palpation of the TMJ capsules was unremarkable
- Palpation of the TM joints (via EAMs) revealed what appeared to be normal function despite the somewhat limited maximum opening
- no evidence of TMJ disc displacement
- Painful paired muscles, normal TM joints, and the report of pain nearly every morning would imply that bruxism (SB) was likely the source of her pain.
- Nonetheless, TMJ imaging will be ordered to make certain that nothing is left to question.
Radiographic Evaluation: TMJ Cone Beam CT Images
- Figure 5 shows EJ’s TM joints from a sagittal perspective
- These cone beam images were read by a board-certified radiologist
- The images were described as “normal osseous morphology and condylar position”
- The right condylar process and mandibular ramus were slightly shorter than the left but this was considered a normal variation
- Summary: normal TM joints and apparent normal function
Radiologist Comment on Sinuses and Airway: Perhaps the Missing Link
- The radiologist who read the CBCT images made very interesting comments under the “Sinuses and Airway” which, in the absence of overt TMJ disease, compelled me to approach this “tooth grinding” and “pain upon-awakening” case as symptoms secondary to a SRBD
- Above you will see a portion of the final comments made by the radiologist regarding the size of EJ’s oropharyngeal airway.
- Figure 6 is for comparative purposes contrasts the A-P dimension of a normal sized airway to a subnormal sized airway
- It is easy to see that EJ’s airway is grossly subnormal in size and a definitive risk for SRBD; a likely contributing factor to sleep bruxism and orofacial pain.
Looking More Closely: Intraoral Risk Factors for SRBD
- Figure 8 is an intraoral view of Ej’s mouth
- The soft tissue appearance seen in EJ are risk factors for SRBD, specifically:
- narrow and deep palate,
- coated and scalloped tongue and
- a tongue size that seems enlarged compared to the dental arches (Liistro, 2003)
Looking More Closely: Extraoral Risk Factors for SRBD
- Figure 9 accurately portrays EJ’s severe Forward Head Posture (FHP).
- FHP may well represent anatomical differences unique to patients who will/have SRBD. Anatomical factors contributing to the etiology of OSA have extensive support in the literature.
- Whether these anatomical variances represent adaptive changes consequent long- standing OSA which has not been addressed, or reflects phenotypic differences of airway morphology, which may predispose one to developing a SRBD, is debatable.
- Nonetheless, it is important to know the predominant anatomic alterations in individuals with apnea, so that health care professionals can identify the risk factors and refer the patients for proper diagnosis and treatment (Piccin, 2016)
Hypothesis: Address EJ’s Apparent SRDB which will Reduce Microarousals which Cause Her SB
- Figure 10 shows EJ habitually has her mouth open during the day; perhaps more easily appreciated by looking back at Figure 9 – side view.
- Daytime mouth breathing is more common among patients who may have SRBD and screening is advised in order rule out a problem (Detailleur, 2017)
- This “condition” or habit, is perhaps a bit less obvious risk factor for SRBD but given EJ’s past medical history, it took on more significance as we were developing this case
Treating EJ: Fixing Her Airway and Her Pain… and Much More!
Addressing EJ’s pain complaints by addressing what appears to be a SRBD was made and well supported by clinical evidence presented herein and current literature (Lavigne, 2007); (Smith M. W., 2009).
We decided to provide EJ not with a single arch TMJ splint but a Mandibular Advancement Device (MAD), specifically a Myerson EMA® (Figure 11) because the design is an elegant solution to controlling the cause of her pain: SRBD which leads to sleep bruxism.
The Myerson EMA® by design, lends itself nicely to managing these sorts of TMD/Sleep cases which I suspect are far more prevalent in our practices than current literature might suggest.
The EMA® (Figs. 11-14) is a two-part appliance consisting of an upper tray and separate lower tray; the trays are connected by elastic straps on either side called Durometers® .
When both trays are connected keeping the mandible advanced while sleeping, it is very effective to do what it was originally designed to do…maintain a patent airway while sleeping or more specifically control obstructive sleep apnea (Figure 11).
Another very useful feature of this particular MAD is that the trays can be easily separated and the mandibular tray can be worn independently for daytime use for preventing disc displacement. In the case of EJ, it also served as a habit-control device specifically for helping to reduce daytime bruxism which we found to be instrumental in helping to control her daytime pain.




A Surprise Ending
EJ was provided with the EMA® and she was very compliant with my request to wear the lower tray during the day and the dual appliance (both attached) while sleeping.
I was very happy to hear, after only a week or so, that her symptoms were rapidly resolving. It was not many weeks into treatment when her aunt (who was also her guardian) began to accompany EJ to her follow-up progress evaluations. She wanted to express her happiness with just how much better EJ was doing symptomatically, declaring how much her pain had declined and how much less she was now awakening at night because she was no longer having to “wake up all night to go to the bathroom.”
Treatment progressed very well, and I kept EJ in treatment for approximately one year. After twelve months, we reduced the use of her EMA® to nighttime only and EJ continued to do very well. It was remarkable how animated and happy she was each time she returned for a follow up visit. So much improved, that now she was working as a volunteer “every week, part-time.” Her aunt told me that she had not been able to hold any sort of a job for years because of her “health problems”…not much more was said at that time.
It would be approximately 15 months since she began therapy, that we learned more about her life before the EMA®. I learned that EJ had been medically disabled due to her uncontrolled epilepsy since age 10.
EJ and her aunt went on to tell us that from the very first night that she wore the EMA® that she has NOT HAD A SINGLE SEIZURE! Which is why she was now able to keep a job for the first time ever in her life. Also, she informed us that her neurologist had begun to withdraw her AEDs, one-by-one, and that instead of five AEDs, she was now only taking two, and it was her neurologist’s goal to withdraw her from ALL her AEDs by the end of this year (2019).
Hearing this, I decided to refer EJ for a polysomnogram to better understand perhaps how fragmented sleep might explain the genesis of her prior-to-MAD uncontrolled epilepsy. EJ had a previous PSG but it was interpreted as “inconclusive”. We ultimately obtained a copy of all available medical records from the time that she had been diagnosed with epilepsy. The PSG report I saw was only a summary and did not provide an index of respiratory-related arousals. I did request that esophageal manometry (aka: PES) be applied during her upcoming PSG because given her past medial history, even non-apneic events from increased “effort” of breathing could contribute to sleep fragmentation, which we want to keep to a minimum. If her EMA cannot fully resolve her SRDB, I will suggest combination therapy, i.e. CPAP + her EMA.
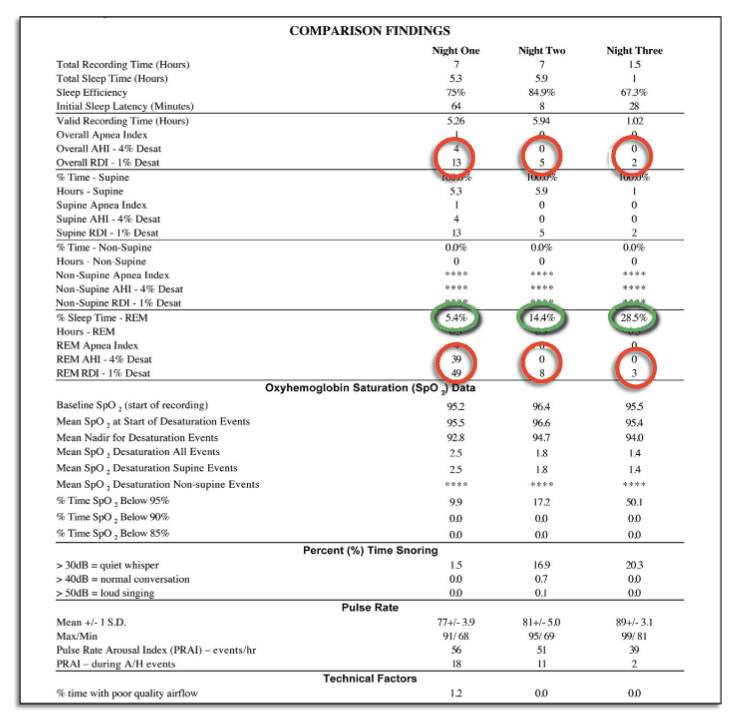
While waiting for her PSG, we provided EJ with a Home Sleep Test Monitor (HST – ARES Watermark brain monitor) to determine if she had a SRBD. We were clear with EJ that the results of this 3-day HST trial would not constitute a diagnosis and that only a certified sleep specialist could make a final diagnosis. EJ understood that regardless of the outcome, that a referral for an attended PSG was indicated. We provided EJ the HST for three successive nights. She was instructed to withdraw the EMA® for night #1, but nights #2 and #3, she would use the EMA as she always had.
You can see from the results below in figure 15, that there certainly appears to be significant breathing-related sleep fragmentation on night #1 and that on nights #2 and #3, that the fragmentation is appreciably reduced to nearly zero. I will not attempt to interpret the HST report but the improvement in respiratory indices is quite obvious.
Why is This Case Report Important?
A review of current medical literature exploring sleep disorders and childhood epilepsy is aptly summarized in a report of a study performed at the University of Calgary “… children with epilepsy had significantly greater sleep problems than their non-epileptic siblings….” (Wirrell, 2005). The conclusion seems to reflect selection bias that sleep problems and epilepsy are unidirectional or simply stated that seizure disorders are a risk factor for pediatric sleep problems. The case report presented here would suggest something quite contrary: that there is a bi-directional relationship between pediatric sleep problems and epilepsy, that an unaddressed SRBD is a risk factor for refractory pediatric epilepsy.
A bi-directional correlation between pediatric sleep problems and epilepsy is anathema to the bulk of current scientific literature that views the degradation of sleep quality which is common to most epileptics as merely a co-morbidity of the epilepsy, i.e. that it is a uni-directional correlation. Again, I feel that is a demonstration of selection bias against SRBD as possibly etiologic solely because of the minimal education of healthcare professionals on the subject of sleep-disordered breathing as previously stated.
Concluding Remarks

I learned a great deal from this case. It was interesting that a significant percentage of cases of epilepsy in children remains idiopathic (Berg, 2001) which could mean that the inherent bias from a lack of sufficient education in sleep disorders is preventing their clinicians from including SRBD in their differential diagnosis. This was clearly the case with EJ because, despite the effort of her doctors to treat her epilepsy, it remained refractory to medication. No one noticed that all of her seizures occurred WHILE SHE WAS SLEEPING and thought to pursue a thorough sleep assessment.
I feel that it was my education in sleep medicine/dental sleep medicine that enabled me to understand the more subtle aspects of EJ’s case, much to her benefit. My goal was to reduce her daily pain. To do so it meant I had to control her sleep-related bruxism. I suspected a SRBD triggered her bruxism. The radiology report plus data that shows women with polycystic ovary syndrome (another of EJ’s medical problems) have 30x the risk for SRBD, clearly supported my clinical impression that her TM “J” problem paled in comparison to her airway problem (Kato, 2001). The evidence guided our clinical decisions so the choice to employ the EMA to help her with her pain was simple, logical, and based on evidence.
Limitations of this case: It is a single case without controls. Because of EJ’s life-changing outcome, the significance of the implications of this case report cannot be overstated. It is our plan to develop and initiate a randomized controlled crossover trial may be of great benefit to prove or disprove the hypothesis that sleep fragmentation is a risk factor for refractory epilepsy and can be treated with mandibular advancement devices (Selye, 1956) (Gold, 2011).
References
- Aschengrau, A. a. (2013). Essentials of epidemiology in public health. ones & Bartlett Publishers.
- Bailey, D. a. (2010). Oral appliance therapy in sleep medicine. Sleep Medicine Clinics, 5(V), 91-98.
- Berg, A. S.-R. (2001). Defining early seizure outcomes in pediatric epilepsy: the good, the bad and the in-between. . Epilepsy Research, 43(1), 75-84.
- Detailleur, V. B. (2017). Are Sleep Disordered Breathing Symptoms and Maxillary Expansion Correlated? A Prospective Evaluation Study. Journal of Sleep Disorders: Treatment and Care.
- Elliott, R. E. (2011). Vagus nerve stimulation in 436 consecutive patients with treatment-resistant epilepsy: long-term outcomes and predictors of response. Epilepsy & behavior, 20(1), pp. 57-63.
- Gjevre, J. T.-G. (2013). Inter-observer reliability of candidate predictive morphometric measurements for women with suspected obstructive sleep apnea. Journal of Clinical Sleep Medicine, 9(07), pp. 695-699.
- Gold, A. (2011). Functional somatic syndromes, anxiety disorders and the upper airway: a matter of paradigms. Sleep medicine review, 15(6), pp. 389-401.
- Jonas, D. A. (2017). Screening for obstructive sleep apnea in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA, 317(4), 415-433.
- Kato, T. R. (2001). Sleep bruxism: an oromotor activity secondary to micro-arousal. (.. ,.-1. ., Ed.) Journal of dental research, 80((10)), 1940-1944.
- Kryger, M. R. (1996). Utilization of health care services in patients with severe obstructive sleep apnea. Sleep, 19(suppl_9), S111-S116.
- Lavigne, G. H. (2007). Genesis of sleep bruxism: motor and autonomic-cardiac interactions. Archives of oral biolog, 52(4), 381-384.
- Levendowski, D. M. (2008). Prevalence of probable obstructive sleep apnea risk and severity in a population of dental patients. Sleep and Breathing, 12((4)), 303-309.
- Liistro, G. R. (2003). High Mallampati score and nasal obstruction are associated risk factors for obstructive sleep apnoea. European Respiratory Journal, 21(2), 248-252.
- Malow, B. L. (2000). Obstructive sleep apnea is common in medically refractory epilepsy patients. Neurology, 55((7)), 1002-1007.
- Mold, J. Q. (2011). Identification by primary care clinicians of patients with obstructive sleep apnea: a practice-based research network (PBRN) study. The Journal of the American Board of Family Medicine, 24((2)), 138-145.
- N. Aprahamian, M. H. (2014). Pediatric first time non-febrile seizure with focal manifestations: Is emergent imaging indicated? Seizure, 23(9), 740-745.
- Olmos, S. (2016). Comorbidities of chronic facial pain and obstructive sleep apnea. Current opinion in pulmonary medicine,, 22(6), 570-575.
- Piperidou, C. K. (2008). Influence of sleep disturbance on quality of life of patients with epilepsy. Seizure, 17((7)), 588-594.
- Ramar, K. D. (2015). Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. Journal of clinical sleep medicine, 11((07)), 773-827.
- Rosen, R. Z. (2001). Low rates of recognition of sleep disorders in primary care: comparison of a community-based versus clinical academic setting. Sleep Medicine, 2((1)), 47-5.
- Selye, H. (1956). The stress of life.
- Smith, M. W. (2009). Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep, 32(6), 779-790.
- Smith, M. W. (2009). Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep, 32((6)), 779-790.
- Sorscher, A. (2008). How is Your Sleep: A Neglected Topic for Health Care Screening. The Journal of the American Board of Family Medicine, 21((2)), 141-148.
- Speltz, L. (2014). Assessing First Seizures in Children and Adolescents. A Pediatric Perspective, 23(1), VOLUME, NUMBER.
- Stores, G. (2007). Clinical diagnosis and misdiagnosis of sleep disorders. Journal of Neurology, Neurosurgery & Psychiatry, 78((12)), 1293-1297.
- Stores, G. (2009). Errors in the recognition and diagnosis of sleep disorders. Progress in Neurology and Psychiatry, 13((6)), 24-33.
- Wirrell, E. B. (2005). Sleep disturbances in children with epilepsy compared with their nearest-aged siblings. Developmental medicine and child neurology, 47(11), 754-759.