
Do you have patients with worn teeth? Do you know what to say to them? A growing set of patients with tooth damage can be helped as a result of a new class of Electromyographic (EMG) testing. Surface EMG testing has been available for many years but it records only a portion of the problem. Other critical variables must be measured in conjunction with the surface EMG to capture data the dentist needs to accurately triage and treat patients who present with puzzling conditions.
Parafunctional EMG (PEMG) should include surface EMG of the masseter measured while the patient sleeps and also include a detailed evaluation of the airway on a single time axis which establishes not only the presence of the PEMG activity but also the context in which these damaging events occur.
A growing set of patients with tooth damage can be helped as a result of this new class PEMG testing. Adding to the PEMG landscape is calibrating the signal for the purpose of quantifying the amount of energy exerted by the masseter muscles. Knowing the frequency of the PEMG events as well and the strength and magnitude of the PEMG events is the final component we believe will enable the clinician to more effectively treat patients with damaging bruxism.
Bio-mechanical measuring technology has advanced to the extent that we can routinely collect PEMG and airway data on a single time axis to create invaluable information when used by trained individuals. The implication is with updated training and the ability to create the PEMG landscape the dentist can improve long term treatment and rehabilitation outcomes on patients which often seemed hopeless in the past.
First let’s talk about EMG. The masseter muscles are particularly busy muscle participating in many essential tasks, especially during sleep. Swallowing and yawning and a variety of other relatively normal and mundane activities are accompanied by lessor-known activities (Figs. 1-2), such as Rhythmic Masticatory Muscle Activity, (RMMA — essentially twitches during sleep), associated with arousals and changes in sleep stages.
To summarize the challenge there are several types of EMG waveforms we measure many of which are of little or no concern. Distinguishing those from the more clinically significant waveforms such as those generated during a clench or a grind can prove challenging.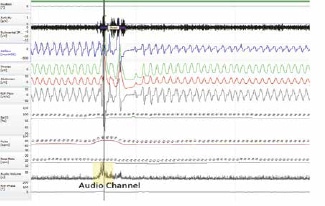
Further complicating the effective assessment of parafunctional EMG activity is the lack of information on the strength or magnitude of the clinically significant waveforms seen during clenches in particular. There are a number of occlusal mappers which can identify mal-occlusions and highlight the damaging contact points but these tests are typically performed while awake sitting in a dental chair and not while the patient sleeps. One of the specific technology advancements which has facilitated the assessment of parafunctional activity is the ability to record the audio and convert the audio recording to a waveform. By identifying the distinctive sound of tooth to tooth contact, we can determine which muscle activities are significant and which are not. Many of us know this unique sound and find it difficult to listen to. For the same reason it is easy to identify in the audio recording (Fig. 3).
So the task of quantifying damaging parafunctional activity is challenging but not insurmountable. By creating specific algorithms to detect normal activity, ignore artifacts and quantify the remaining significant parafunctional activity, we have made the first step to measure bruxism effectively.
To quantify bruxism we need to calibrate the surface EMG signal. This establishes a baseline energy unit by performing a waking “clench”. We ask our patients to bite down as hard as the can five times (Fig. 4).
These clenches are accurately measured and used to create the patient’s “Energy Unit (eU).” Through this process the total energy expended by the masseter is quantified as well as the total clench energy (Fig. 5). It is important that this is custom-generated by each patient, rather than comparing their test results to some population-generated ‘normal values.’
The other major challenge is to cast the bruxism data in the proper context of what else is going on while the patient sleeps. By comparing timing of airway events and muscle activity, we can draw some conclusions about correlation of these events. The goal is to accurately quantify the significant bruxism in the context in which they occur.
The first example most of us think of is a clench occurring after an obstructive apnea or hypopnea which I call Post Arousal Clench, (PACL). In the example below we suspect tooth contact due to the audible signal detected timed with the clench (Figs. 6-8).
The value of this assessment technique is the ability of the dentist, armed with more specific information, to plan for a more tailored treatment or rehabilitation. Bruxism has been an enigma since the first time anyone noticed a worn tooth. Showing what appears to be a compromised airway correlation may unlock a bit of the mystery and put more previously ‘difficult’ cases on an effective treatment path.


It’s difficult to say but many patients in the dental chair may not be receiving the most effective protection against bruxism. For example should a patient be fitted for a night guard which has been shown to introduce risk to the airway or an appliance which takes into account the patient airway condition?
So to answer the question: “Why Measure for Parafunctional EMG Activity?” Provide vital information to the treating dentists to more accurately categorize their patient’s condition, thus allowing them to choose the best therapy, and thereby improve outcome. Isn’t that the goal of all medicine?
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..

